Incorrect Gender and Diagnosis Codes
The Impact of Incorrect Gender and Diagnosis Codes in Medical Billing
Summary:
Submitting incorrect diagnoses and gender identifiers with a medical claim to a payer leads to a whole host of easily avoidable problems for claims processing, check-runs for payers, collection payout timeframes for clinics, HEDIS scores for providers, and even exclusion of providers from current plans if done continually, and most importantly inaccurate patient records which can affect the speed and accuracy of current and future patient treatment outcomes.
What is HEDIS?
HEDIS (Healthcare Effectiveness Data and Information Set) scores are a widely used measure of healthcare quality that is used by health plans to assess the performance of healthcare providers. With more than 90 measures across 6 domains of care including:
- Effectiveness of care
- access/availability of care
- Experience of care
- Utilization and Risk Adjusted Utilization
- Health Plan Descriptive Information
- Measures Reported using Electronic Clinical Data Systems
Inaccurate diagnosis and gender information can have a significant impact on the HEDIS scores, affecting the performance ratings of healthcare providers
Incorrect Diagnosis Impact
Submitting claims with the wrong diagnosis information can have a negative impact on the HEDIS scores of healthcare providers. The HEDIS measures are designed to evaluate the quality of care provided to patients based on specific clinical guidelines. Inaccurate diagnosis information can lead to the misclassification of patients and the failure to properly identify patients who require specific care. This can lead to a lower overall score for the healthcare provider, as well as a lower score for the specific HEDIS measure related to misdiagnosis.
For example, consider the HEDIS measure related to the management of
hypertension. This measure evaluates the percentage of patients with hypertension who have their blood pressure controlled to a specific level. If claims are submitted with an incorrect diagnosis of hypertension, then patients who should receive care for hypertension may not be identified, and the healthcare provider's score for this measure may be lower than it should be. Similarly, if claims are submitted with an incorrect diagnosis of diabetes, then patients who require diabetic care may not receive the necessary care, and the healthcare provider's score for the HEDIS measure related to diabetes care may be negatively impacted.
| Measure Year | Commercial HMO | Commercial PPO | Medicaid HMO | Medicare HMO | Medicare PPO |
|---|---|---|---|---|---|
| 2021 | 60.3 | 50.8 | 58.6 | 70.4 | 70.1 |
| 2020 | 51.8 | 46.2 | 55.9 | 63 | 61.8 |
| 2019 | 62.1 | 47.6 | 60.8 | § | § |
| 2018 | 61.3 | 48.8 | 58.9 | 69.7 | 68.8 |
Table Reference:
https://www.ncqa.org/hedis/measures/controlling-high-blood-pressure/
Incorrect Gender Coding Impact
Submitting claims with incorrect gender information can also have a significant impact on the HEDIS scores of healthcare providers. HEDIS measures are often gender-specific, such as the measure related to breast cancer screening for women or the measure related to prostate cancer screening for men. If claims are submitted with incorrect gender information, then the healthcare provider's score for the corresponding HEDIS measure may be negatively impacted.
For example, consider the HEDIS measure related to breast cancer screening for women. This measure evaluates the percentage of women who have received a mammogram within a specific time frame. If claims are submitted with incorrect gender information, then men may be incorrectly included in the denominator for this measure, resulting in a lower score for the healthcare provider. Similarly, if claims are submitted with incorrect gender information for the HEDIS measure related to prostate cancer screening, then women may be incorrectly included in the denominator for this measure, resulting in a lower score for the healthcare provider.
Impact on Healthcare Providers
Submitting claims with incorrect diagnosis and gender information can have a significant impact on the HEDIS scores of healthcare providers. The HEDIS scores are used by health plans to assess the quality of care provided by healthcare providers, and lower scores can result in lower reimbursement rates and decreased patient referrals. Healthcare providers with lower HEDIS scores may also face increased scrutiny from regulatory agencies, which can lead to increased costs and decreased revenue.
In addition to the financial impact, healthcare providers may also face reputational damage if their HEDIS scores are lower than their peers. Lower HEDIS scores may be seen as an indication of lower quality of care, and this can negatively impact patient trust and confidence in the healthcare provider. Healthcare providers may also face increased pressure to improve their HEDIS scores, which can result in increased workload and stress for healthcare providers and their staff.
Local Patient's outlook and family referrals can stop dead in its tracks. If your provider submitted your insurance claim and stated you were a 60-year male who received a pap smear. You probably wouldn’t take them seriously and find another provider, and you surely wouldn’t recommend them to your family members.
Preventing Errors in Diagnosis and Gender Information
To prevent errors in diagnosis and gender information, healthcare providers should implement processes to ensure the accuracy of claims data. Consistently ask your EMR, EHR, and Practice Management vendors to update their cloud hosted applications. If you have a downloaded version on your own server you will need them to send you a file of all new codes and manually update them to remain compliant.
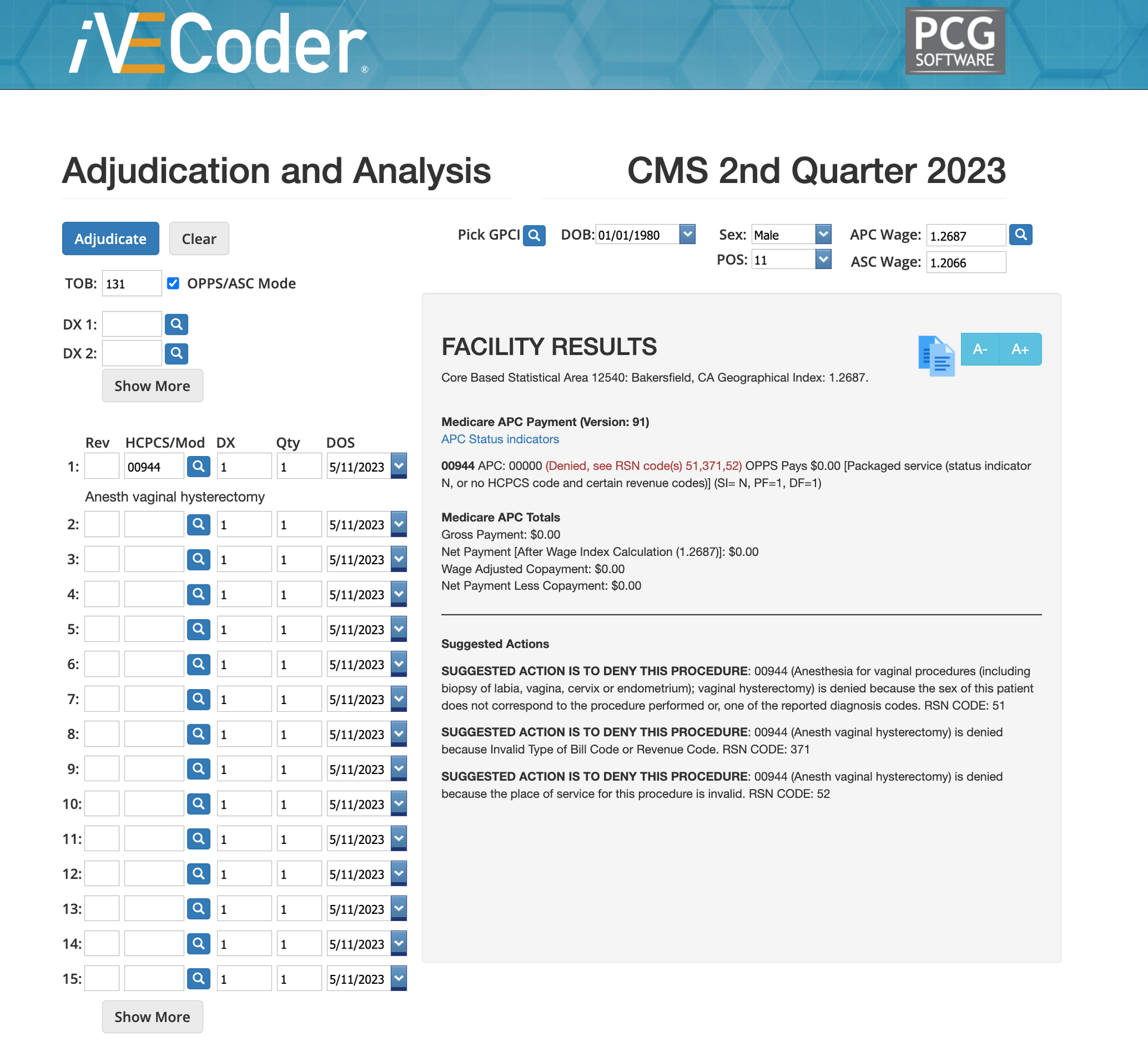
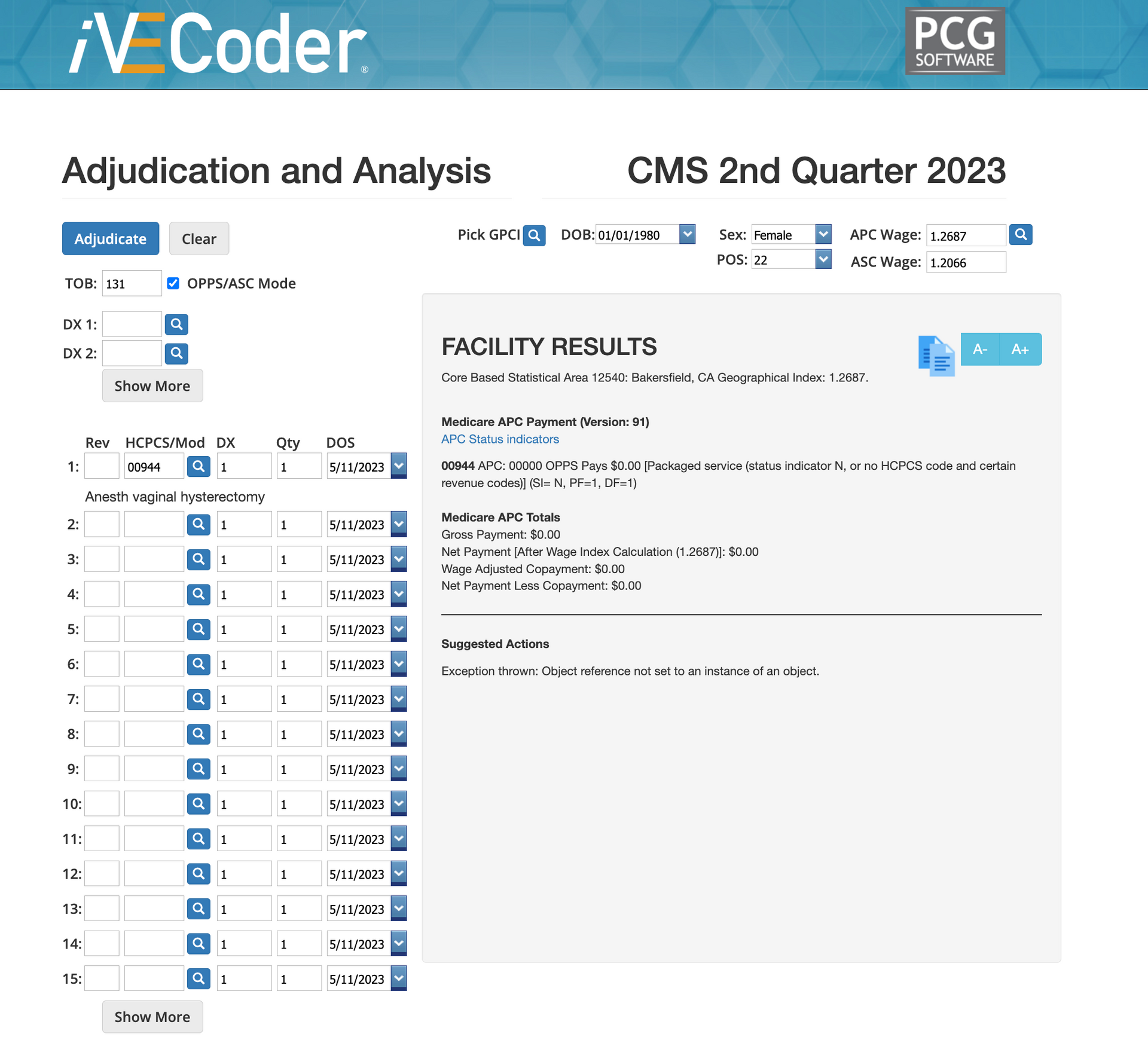
Or there’s a simple way… iVECoder
Run Internal Audits and Increase Compliancy through AI (iVECoder)
Start by running a denial report through your billing software, and find the key codes you continually get denied for. Your plan will not catch everything, but what they do can impact your monthly collections and HEDIS scores as stated above.
At PCG Software, we have a compliance and code lookup tool (iVECoder). That when utilized can help you determine if your claim will likely be approved or denied per CMS and AMA guidelines. It also educates you and your team on which codes can be applied as well as modifiers to genders, places of service, and diagnoses. When you run mock claims you’ll find out why it would be denied and fix it before officially submitting it within your EMR/EHR/Practice Management software. Some of our clients even use iVECoder as a hiring and training tool to ensure their billers and coders know what they’re doing to avoid future patient and financial liability.
See the reasons for a denial before you submit with iVECoder.
Next Steps
In conclusion, submitting claims with incorrect diagnosis and gender information can have a significant impact on the HEDIS scores of healthcare providers. Lower HEDIS scores can lead to financial and reputational damage for healthcare providers, as well as increased regulatory scrutiny. To prevent errors in diagnosis and gender information, healthcare providers should implement processes to ensure the accuracy of claims data and provide ongoing training to their staff. By improving the accuracy of claims data, healthcare providers can improve their HEDIS scores and ensure that they are providing high-quality care to their patients.
IVECoder Information and Plans
Will Schmidt joined PCG Software as their Chief Strategy Officer in November 2022. Prior to PCG, Schmidt lead TNH as their Sr. Vice President to become the 7th largest pharmacy in the nation. He then went on to consult with and serve as Interim CEO or Consultant to over 20 different companies specializing in profit strategies, operational efficiencies, vendor relations and partnerships, and exit strategies, include an international Revenue Cycle Management Company.
Our History and Credibility in Reporting this Information:
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Support Request
New Customer Quick Links
All Rights Reserved | PCG Software, Inc.
Website Created & Managed by Talents Into Profits