Modifier FS - Guide on when, how, and what to use it for
Modifier FS Quick Summary
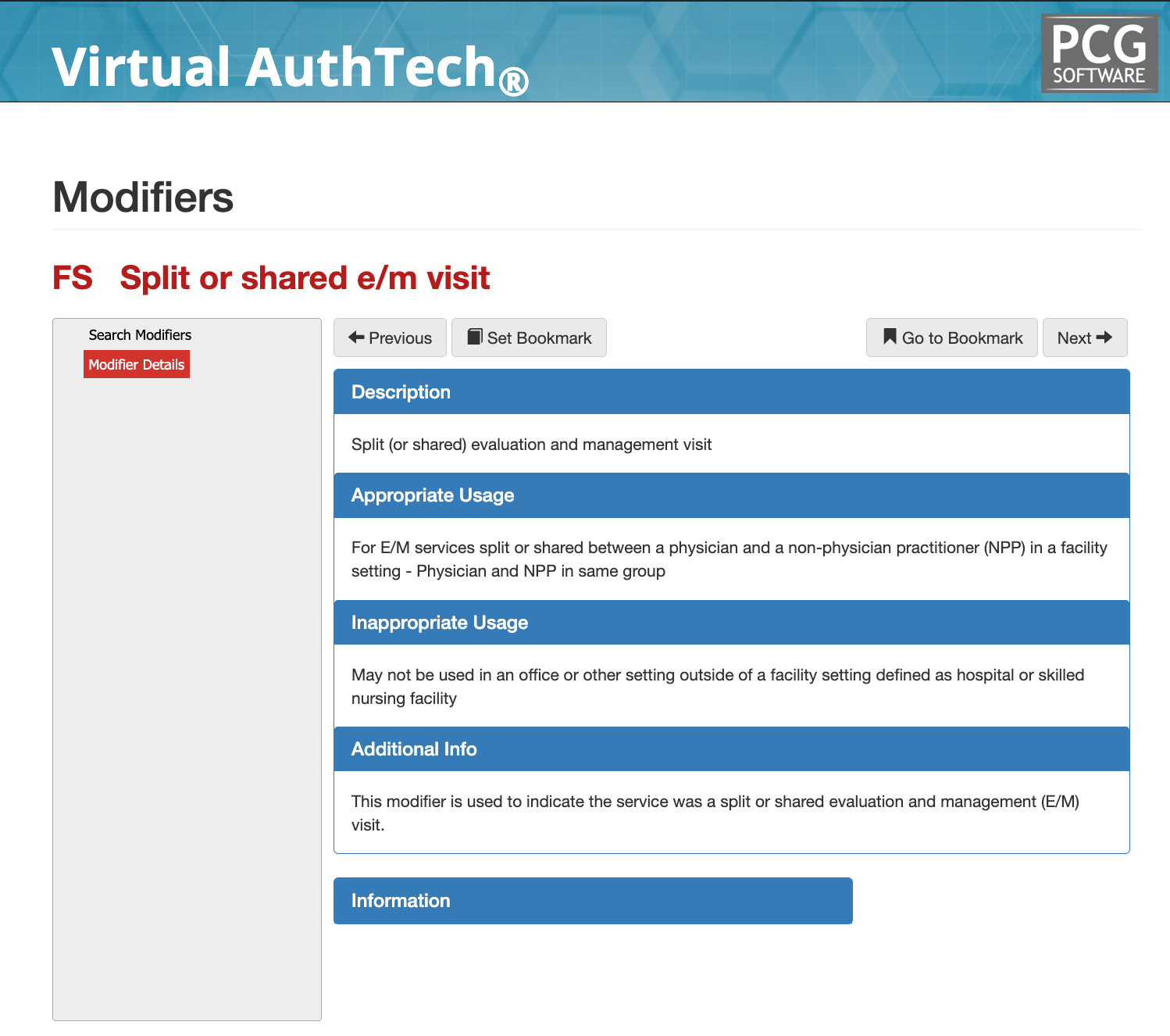
Modifier FS is used to identify split or shared Evaluation and Management (E/M) visits performed jointly by a physician and a non-physician practitioner (NPP) in a facility setting. The modifier communicates to Medicare and other payers that both clinicians participated in the encounter, but that billing is based on the substantive portion of the visit performed by the reporting provider. Modifier FS is primarily a documentation and payment attribution modifier, not a bundling or sequencing modifier, and is subject to strict CMS rules implemented beginning in 2022.
Modifier FS Description & Usage
Modifier FS indicates that an E/M service was split or shared between a physician and an NPP who are part of the same group practice and who provided care to the same patient on the same calendar date in a facility setting. The modifier applies only to E/M services reported under Medicare Part B and is intended to ensure accurate attribution of work, compliance with scope-of-practice rules, and correct payment determination.
CMS requires that the provider who performs the substantive portion of the visit be the billing provider. The substantive portion is defined as more than half of the total time spent, or, for time-independent codes, the provider who performed all required elements of Medical Decision Making (MDM).
When can I use Modifier FS appropriately?
Modifier FS should be reported when all of the following conditions are met:
- The visit is an E/M service eligible for split or shared billing.
- The service occurs in a facility setting, such as a hospital inpatient unit, hospital outpatient department, emergency department, or skilled nursing facility.
- Both a physician and an NPP from the same group participate in the visit.
- The physician or NPP performs the substantive portion of the service.
- Documentation clearly supports shared involvement and substantive work attribution.
Modifier FS does not change payment rates by itself, but signals to CMS that split/shared rules were applied and substantiated.
Example 1: Hospital Inpatient Split Visit Based on Time
A physician assistant evaluates an inpatient in the morning, reviews labs, and documents an assessment. Later the same day, the physician performs an exam, updates the treatment plan, and spends more than half of the total encounter time managing the patient. Because the physician performed the substantive portion based on time, the E/M service is billed under the physician with Modifier FS appended.
Modifier FS and Facility-Only Restrictions
Modifier FS is restricted to facility settings only. CMS explicitly prohibits the use of Modifier FS in non-facility environments, including physician offices, freestanding clinics, and other outpatient settings not defined as facilities under Medicare rules. Split or shared E/M services performed in an office setting must follow the incident-to rules instead, and Modifier FS must not be reported in those cases.
Example: Office Visit Not Eligible for Modifier FS
A nurse practitioner and physician both see a patient in a private office setting on the same day and contribute to the visit. Even if the physician performs the substantive portion, Modifier FS is not permitted because the encounter did not occur in a facility. The service must be billed according to standard office E/M or incident-to rules without Modifier FS.
When is it not appropriate to use Modifier FS?
Modifier FS should not be reported in the following situations:
- The service occurs in an office or other non-facility setting
- Only one provider performed the E/M service
- The physician and NPP are not in the same group practice
- The visit does not qualify as an E/M service
- Documentation does not clearly establish the substantive portion
- The modifier is used to bypass supervision or scope-of-practice rules
Use of Modifier FS without meeting CMS conditions is a common trigger for medical review and recoupment.
Example: Incomplete Documentation of Substantive Portion
A physician and NPP both document brief notes for the same inpatient visit, but neither record clearly establishes who performed the substantive portion. Because CMS requires explicit attribution, Modifier FS is inappropriate and the claim is vulnerable to denial or downcoding.
Documentation Requirements for Modifier FS
Strong documentation is essential for Modifier FS compliance. The medical record must clearly establish:
- Both providers’ participation in the encounter
- The total time spent by each provider or clear MDM attribution
- Which provider performed the substantive portion
- The facility setting where the service occurred
- Alignment with CMS split/shared rules effective in 2022 and later
Documentation must support why the billing provider qualifies as having performed the substantive portion. Statements such as “shared visit” without time or MDM clarity are insufficient.
Example: Proper Substantive Portion Documentation
An inpatient progress note includes separate entries from the NPP and physician, with time clearly documented for each. The physician’s note confirms they spent more than half of the total encounter time managing the patient’s care. The service is billed under the physician with Modifier FS, supported by compliant documentation.
Helpful tips on Modifier FS
Modifier FS and Adjudication Logic
From a payer adjudication perspective, Modifier FS functions as a compliance signal, not a payment enhancer. Claims systems use the modifier to identify split/shared services and route them for validation of time, MDM, provider type, and setting.
CMS and Medicare Administrative Contractors review Modifier FS claims closely to ensure:
- The service occurred in a qualifying facility
- The billing provider performed the substantive portion
- The visit was not improperly billed as shared to maximize reimbursement
- Documentation supports shared involvement without duplication
Modifier FS claims lacking defensible documentation are unlikely to survive automated edits or manual review.
Compliance Considerations for Modifier FS
Modifier FS represents a high-risk modifier due to its reliance on time-based or MDM-based attribution and its frequent misuse outside facility settings. Health plans and CMS auditors closely monitor split/shared billing patterns for improper supervision, upcoding, and scope-of-practice violations. Repeated misuse may trigger broader E/M audits, provider education requirements, or repayment demands. Organizations should implement clear internal policies, provider education, and documentation standards to ensure Modifier FS is applied sparingly, intentionally, and only when CMS requirements are fully met.
Summary on Modifier FS
Modifier FS is designed to support compliant billing of split or shared E/M visits in facility settings when both a physician and NPP participate in patient care. It does not change payments on its own, but it plays a critical role in payment attribution and compliance enforcement. When used correctly, Modifier FS ensures transparency, aligns with CMS rules, and supports accurate reimbursement. When used incorrectly, it is a frequent source of denials, audits, and payment recoveries. Understanding the distinction between facility and non-facility settings, substantive portion rules, and documentation expectations is essential for compliant Modifier FS reporting.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
Free Payer Claims Audit
Complete the form, and we'll contact you to schedule an introductory meeting and discuss our FREE 3-year claims audit to identify areas for cost containment and compliance.
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others