Understanding CPT Code 99213
CPT 99213 Summary:
The 99213 CPT code is a commonly used code in the healthcare industry. It plays a crucial role in documenting and billing for medical services provided during an office visit. Understanding the 99213 CPT code and its significance is essential for healthcare professionals, medical coders, insurance providers, and patients alike.
The CPT code system is a standardized set of codes used to describe medical procedures and services rendered by healthcare providers. It was developed by the American Medical Association (AMA) to ensure uniformity and accuracy in documenting and billing for medical services. CPT codes serve multiple purposes, including facilitating communication between healthcare professionals, enabling accurate billing and reimbursement, and assisting in data collection and research.
The 99213 CPT code specifically represents a level 3 outpatient office visit. It covers a range of services provided by healthcare providers during a standard office visit. These may include evaluation and management services, such as assessing the patient's medical history, conducting a physical examination, diagnosing and treating medical conditions, prescribing medications, and providing counseling or education.
The duration of a typical 99213 office visit can vary depending on the complexity of the patient's condition and the services provided. It is generally considered to be a moderate-length visit that involves a comprehensive assessment and treatment plan.
The 99213 code is used by a wide range of healthcare professionals, including physicians, nurse practitioners, and physician assistants. It is typically used for office visits that require a moderate level of medical decision-making and complexity.
Proper documentation is crucial for supporting the use of the 99213 code. It should include detailed information about the patient's medical history, the nature of the presenting problem, the scope of the examination, the medical decision-making process, and any treatments or interventions provided. Accurate and thorough documentation ensures compliance with coding and billing requirements and facilitates proper reimbursement.
When comparing the
99213 code with other evaluation and management codes, there are key differences in the level of medical decision-making, the complexity of the patient's condition, and the extent of the examination. Healthcare providers must determine the most appropriate code to use based on the specific circumstances of each patient encounter.
Need something faster than a blog about CPT Code 99213?
Understanding the CPT Code System
The understanding of the CPT code system is essential for healthcare professionals. Developed and maintained by the
American Medical Association (AMA), this system allows effective communication between healthcare providers and insurance companies. The key components of the CPT code system include the
CPT Code, category, subcategory, modifiers, guidelines, and updates.
Categories and sub-categories of the CPT Code System
The CPT Code is a unique, five-digit numeric code that represents a specific medical procedure or service. It is categorized and subcategorized for easier identification and billing purposes. Categories in the CPT code system include Evaluation and Management, Anesthesia, Surgery, Radiology, Pathology, and Laboratory, and Medicine.
Subcategories provide a more detailed description of procedures or services within each category. They play a crucial role in refining the coding process and ensuring accurate documentation.
Modifiers are additional two-digit codes that provide extra information about the procedure, such as multiple procedures performed, anatomical location, and time. These modifiers have an impact on billing and reimbursement.
Comprehensive guidelines provided by the AMA for each category and subcategory help ensure consistent and correct code usage. These guidelines assist healthcare professionals in determining the most appropriate code for a specific procedure or service.
The CPT code system is regularly updated to reflect advancements in medical technology, procedures, and practices. It is vital for healthcare professionals to stay updated to ensure accuracy and compliance with the evolving code system.
The understanding of the CPT code system enables healthcare professionals to accurately document procedures, efficiently bill for services, and effectively communicate with insurance companies. By following guidelines and using appropriate codes, healthcare providers ensure proper reimbursement for the services they render. Continuous education and staying up-to-date with the evolving CPT code system is crucial for professionals in the medical field.
Why are CPT codes important in healthcare?
Current Procedural Terminology
CPT codes, also known as Current Procedural Terminology codes, serve a crucial purpose in healthcare. They are a standardized system used to describe medical, surgical, and diagnostic services.
The primary objective of CPT codes is to ensure consistent and accurate documentation, billing, and reimbursement for healthcare services. These codes play a vital role in facilitating communication between healthcare providers, insurance companies, and government agencies, serving as a universal language for medical practices.
By utilizing this standardized coding system, healthcare professionals can effectively communicate the specific procedures and services they provided, streamlining the billing process and ensuring accurate reimbursement.
CPT codes are of utmost importance in properly classifying and identifying medical services, enabling accurate tracking of procedures performed for statistical analysis and research.
These codes aid in determining the appropriate reimbursement level for each procedure, enabling insurance companies to compensate healthcare providers accurately.
The use of CPT codes not only benefits healthcare providers in avoiding billing errors and claim rejections but also benefits patients by helping to coordinate care, maintain accurate records, and streamline billing processes.
It is essential for healthcare providers to understand the purpose of CPT codes, familiarize themselves with relevant codes, and stay updated with any revisions in order to ensure accurate documentation, and billing, maximize reimbursement, and maintain compliance with coding guidelines.
What is the purpose of CPT Codes?
Documentation, Billing, and Reimbursement Quick Overview
CPT codes are crucial in healthcare for standardized and accurate documentation, billing, and reimbursement. Developed by the American Medical Association, these codes describe medical procedures, services, and tests. Here's why CPT codes are important:
1. Effective Communication: CPT codes provide a common language for healthcare providers, insurers, and other stakeholders. They ensure clarity and accuracy when describing procedures and treatments, reducing miscommunication and ensuring everyone understands the services rendered.
2. Billing and Reimbursement: CPT codes are indispensable for accurate billing and reimbursement. They translate medical services into a standardized format easily understood by insurance companies and payers. By using CPT codes, healthcare providers increase the chances of successful reimbursement.
3. Compliance and Auditing: CPT codes ensure compliance with regulatory requirements in healthcare. Accurate coding prevents fraud and facilitates auditing procedures. Healthcare providers can demonstrate compliance and avoid legal issues by maintaining accurate documentation and using the appropriate codes.
4. Data Analysis and Research: CPT codes play a pivotal role in data analysis and research in the healthcare industry. Researchers and stakeholders can gather comprehensive data on specific procedures and services using these codes. This information helps identify trends, evaluate the quality of care, and make informed decisions to improve healthcare delivery.
5.
Cost Management: CPT codes contribute to effective cost management in healthcare. Accurate documentation and coding of procedures allow healthcare providers to track costs associated with specific services. This enables cost analysis, budgeting, and resource allocation, leading to more efficient and cost-effective healthcare delivery.
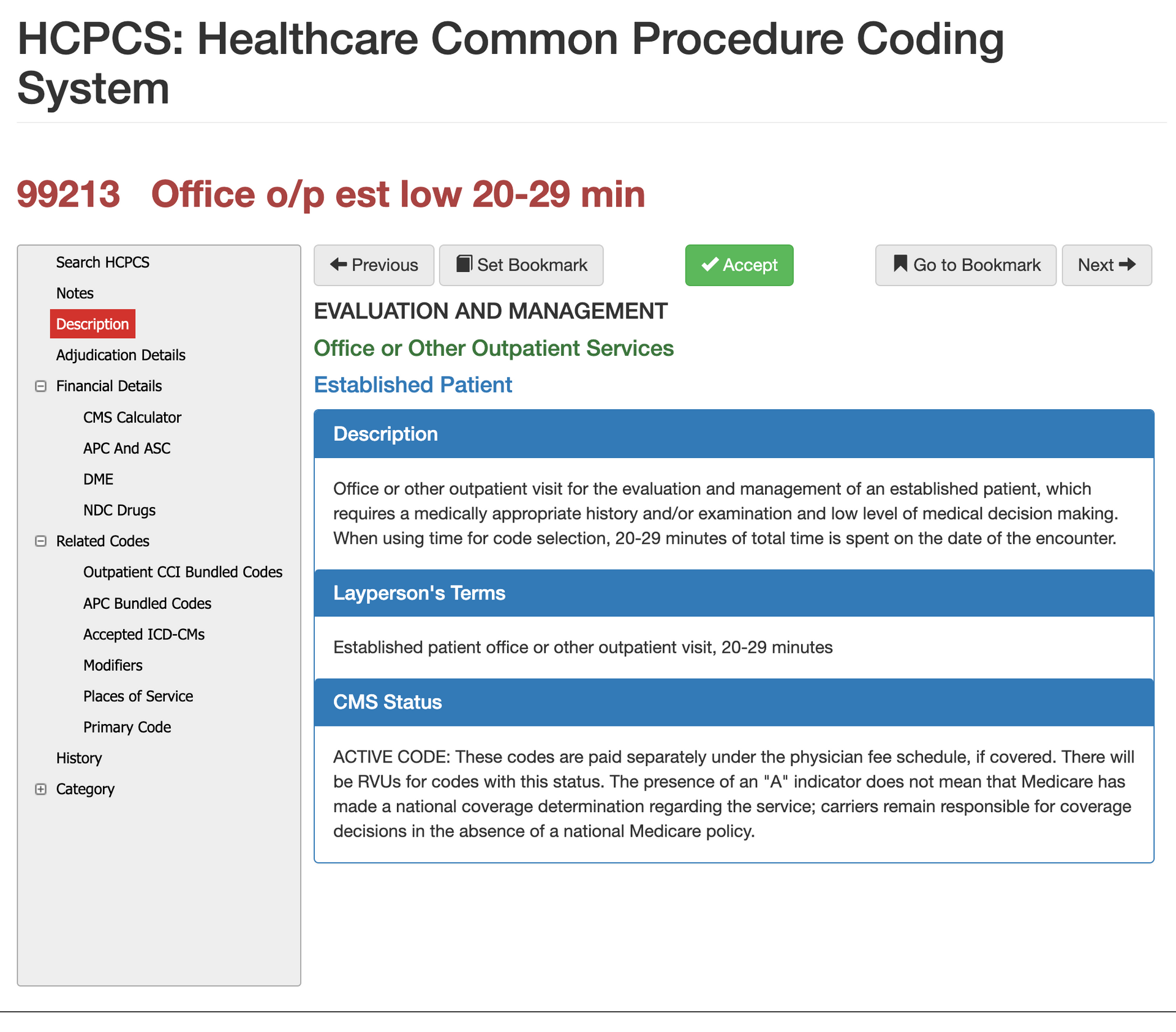
What is the 99213 CPT Code?
The 99213 CPT code is commonly used in medical billing and coding to describe a specific type of outpatient office visit. It represents a moderate level of complexity and evaluation of the patient's condition.
To understand the
99213 CPT code, refer to the following table:
| Code | Level of Complexity | Typical Time | Daignoses |
|---|---|---|---|
| 99213 | Moderate complexity | 20-29 minutes | Common Acute Illnesses |
The 99213 code is associated with a moderate level of complexity and is typically used for office visits that require moderate medical decision-making and management of the patient's condition. These visits usually last around 20-29 minutes.
During a visit with the 99213 code, healthcare professionals often evaluate and manage common acute illnesses such as respiratory infections, urinary tract infections, and minor non-life-threatening injuries.
It's important to note that the specific requirements for using the 99213 code may vary based on organizational or payer guidelines. The level of documentation and medical decision-making required may also differ depending on the patient's needs and the provider's clinical judgment.
Fact: The
99213 code is one of the most commonly used CPT codes for office visits in the United States and accounts for a significant portion of physician encounters.
What does the 99213 CPT Code represent?
The 99213 CPT code represents a medical evaluation and management (E/M) service provided by physicians. This code is used to document and bill for a
level three office visit, which involves a face-to-face encounter with the patient for the evaluation and treatment of a new or existing problem.
Key aspects and components of 99213 CPT Code:
1. Evaluation: The visit includes evaluating the patient's medical history, symptoms, and relevant physical findings. The healthcare professional assesses the patient's condition and determines a treatment plan.
2. Management: The visit focuses on managing the patient's condition. This may involve prescribing medications, ordering diagnostic tests, providing counseling or education, or coordinating with other healthcare providers.
3. Complexity: What does the 99213 CPT code represent? The 99213 code represents a moderate level of complexity. It is used for patients with mild to moderate symptoms or stable chronic conditions requiring ongoing monitoring and management.
4. Time: The typical time spent on a 99213 visit is about 15 minutes. This includes face-to-face time with the patient, reviewing medical records, preparing documentation, and communicating with other healthcare providers if needed.
5. Documentation: Accurate and thorough documentation is essential when using the 99213 code. It should include the reason for the visit, examination findings, treatment provided, and the patient's response to treatment.
Pro-tip: When using the 99213 CPT code, it is important to ensure that the level of complexity and time spent with the patient align with the code's requirements. Detailed and specific documentation will help justify the use of this code and ensure accurate billing.
By understanding what does the 99213 CPT code represent, healthcare professionals can accurately document and bill for their services while ensuring appropriate patient care.
What does CPT Code 99213 cover?
99213 is specifically for office visits, but read to find out details
The 99213 code covers a variety of services provided during an office visit. These services include the evaluation and management of a patient's symptoms or condition, the diagnosis and treatment of minor illnesses or injuries, the prescription or management of medication, the review and interpretation of test results, counseling or education on healthcare issues, and the coordination of care with other healthcare professionals.
The 99213 code is specifically used for office visits that involve moderate medical decision-making and complexity. It is suitable for patients with established conditions or those with new, uncomplicated symptoms. These services encompass a range of primary care services that address the immediate needs of patients.
It is important to note that the 99213 code does not cover more complex procedures or extensive medical evaluations. If a patient requires a higher level of medical decision-making or additional services, a different CPT code may be more appropriate. Therefore, healthcare providers should carefully assess the nature of the visit and use accurate coding to reflect the services provided.
Office Visit duration times for CPT Code 99213
The typical duration of a
99213 office visit is about
15 minutes.
How is the 99213 CPT Code Used?
The 99213 CPT code is commonly used in medical billing and coding for outpatient visits. This code is utilized for a mid-level patient evaluation and management (E/M) service.
Healthcare providers must document the patient's medical history, conduct a problem-focused examination, and develop a treatment plan to support the level of service provided.
So how is the 99213 CPT code used? Well, it is often used for patients with multiple stable chronic conditions or acute uncomplicated illnesses.
It can be billed based on time spent with the patient, where at least half of the total face-to-face time should be devoted to counseling and coordination of care.
It is important to note that reimbursement rates for the 99213 code can vary depending on geographic location and payer.
That's why accurate coding and documentation are crucial for proper billing and reimbursement.
Healthcare providers should carefully assess each patient encounter, document necessary information, and use the appropriate code.
Compliance with coding guidelines and
accuracy in documentation are essential for an effective and efficient healthcare system.
Who uses the 99213 code?
The 99213 CPT code is commonly utilized for billing and documentation in the healthcare industry. It is used by various parties, including healthcare providers, medical coders, insurance companies, government agencies, and patients.
Healthcare providers such as doctors, physicians, and other professionals offering evaluation and management services in outpatient settings frequently rely on the 99213 code. It is particularly prevalent in primary care settings where patients receive routine or episodic care.
Medical coders play a crucial role in assigning the appropriate CPT codes to the services provided by healthcare providers. They possess a strong understanding of the 99213 code to ensure precise billing and reimbursement.
Insurance companies utilize the 99213 code to process claims and determine reimbursement amounts for healthcare providers. By using this code, they can evaluate the complexity and level of service provided during a patient visit.
Government agencies, including Medicare and Medicaid, also depend on the 99213 code. It helps them determine reimbursement rates and guarantee the appropriate utilization of healthcare services.
Although patients do not directly use the 99213 code, they benefit from its implementation. The code assists in standardizing and categorizing medical services, ensuring transparency in billing and reimbursement practices.
It is crucial for all parties involved to understand the correct use and interpretation of the
99213 code to promote fair and accurate billing practices. By effectively utilizing this code, healthcare operations become more efficient, reimbursement becomes appropriate, and patient satisfaction improves.
How does the 99213 code impact insurance billing and reimbursement?
Understanding how the 99213 code impacts insurance billing and reimbursement is crucial for healthcare providers. Here are some key points to consider:
1. Insurance coverage: Most insurance providers, including Medicare and Medicaid, recognize the 99213 code. This means that services billed under this code are more likely to be covered by insurance.
2. Reimbursement rates: The reimbursement rates for the 99213 code vary depending on the insurance plan and location. On average, healthcare providers can expect to receive between $70 and $100 for an office visit billed under this code.
3. Documentation requirements: Healthcare providers must accurately document the services provided during the office visit to ensure proper reimbursement. This includes details like the patient's complaint, history, examination findings, and decision-making. Meeting these requirements justifies the use of the 99213 code for billing purposes.
4. Coding accuracy: Accurately assigning the 99213 code to office visits is crucial. Using the wrong code can lead to claim denials or reduced reimbursement. Providers should ensure that the services provided during the visit meet the specific criteria outlined by the 99213 code.
5. Impact on revenue: Proper use of the 99213 code can significantly impact a healthcare provider's revenue. Accurately documenting and coding office visits using this code optimizes reimbursement and revenue.
6. Claim submission: Healthcare providers must submit claims for services billed under the
99213 code to insurance companies for reimbursement. This involves providing necessary documentation and coding information. Timely and accurate claim submission ensures prompt reimbursement.
Understanding the Documentation Requirements for the 99213 Code
The 99213 code is important in medical billing. To code accurately, understanding the documentation requirements for the 99213 code is essential. Here is what you need to know:
- Medical necessity: Document the medical necessity of the visit to support using the 99213 code. There must be a legitimate reason for the patient encounter, like an illness, injury, or ongoing condition.
- Established patient: Use the 99213 code for patients who received medical services in the past three years.
- Level of complexity: The 99213 code represents an intermediate level of complexity for evaluation and management services. The documentation should reflect this complexity and include details about the patient's medical history, examination, and decision-making.
- Time-based documentation: The 99213 code can also be determined based on the time spent with the patient. The provider should spend at least 15 minutes face-to-face with the patient, with most of that time dedicated to medical decision-making.
- Relevant documentation: To support the 99213 code, include pertinent information such as the reason for the visit, history of present illness, review of systems, physical examination, assessment, and plan of care.
Pro-tip: Healthcare providers should establish guidelines and templates to streamline the documentation process for accurate and complete understanding the documentation requirements for the 99213 code documentation. Regular training and education for staff can improve understanding and compliance with the requirements.
By understanding the documentation requirements for the
99213 code, healthcare providers can accurately code, bill, and comply with coding guidelines to ensure appropriate reimbursement.
What type of documentation is necessary to support the use of the 99213 code?
To support the use of the 99213 code, specific documentation is necessary. This documentation ensures accurate billing and reimbursement. Here are the key types of documentation required:
- Medical history: Include relevant details about the patient's past medical history, including any chronic conditions or previous treatments.
- Chief complaint: Clearly document the patient's reason for the visit, including specific symptoms or concerns.
- Physical examination: Perform and document a thorough physical examination, including vital signs, examination of specific body systems, and any additional tests or procedures conducted.
- Diagnosis or assessment: Clearly document the provider's diagnosis or assessment of the patient's condition based on the information gathered during the visit.
- Treatment plan: Outline the proposed treatment plan, including medications prescribed, referrals made, or follow-up tests or visits recommended.
- Time spent: Document the amount of time spent on the evaluation and management of the patient's condition. The 99213 code represents a low to medium complexity visit that typically requires a minimum of 15 minutes of physician time.
By including all of these elements in the documentation, healthcare providers can support the use of the 99213 code and accurately reflect the level of service provided to the patient. This documentation is essential for proper billing and reimbursement, as it provides evidence of the medical necessity and complexity of the visit.
What are the key elements that should be included in the documentation?
Key elements in the documentation for the 99213 CPT Code should include:
Chief complaint: State the reason for the patient's visit.
-
History of present illness (HPI): Describe the details of the patient's current symptoms or condition.
Past medical, family, and social history: Include relevant information about the patient's medical background, family medical history, and social habits.
Review of systems (ROS): Assess the patient's various body systems for any additional symptoms or concerns.
Physical examination findings: Provide objective findings from the physical examination.
Medical decision making (MDM): Explain the thought process behind diagnosis and treatment decisions.
Time spent with the patient: Document the total time spent on the encounter.
Pro-tip: When documenting for the 99213 code, ensure the information is relevant and supports the medical necessity of the visit. Thorough documentation aids in accurate coding, billing, and effective communication among healthcare providers.
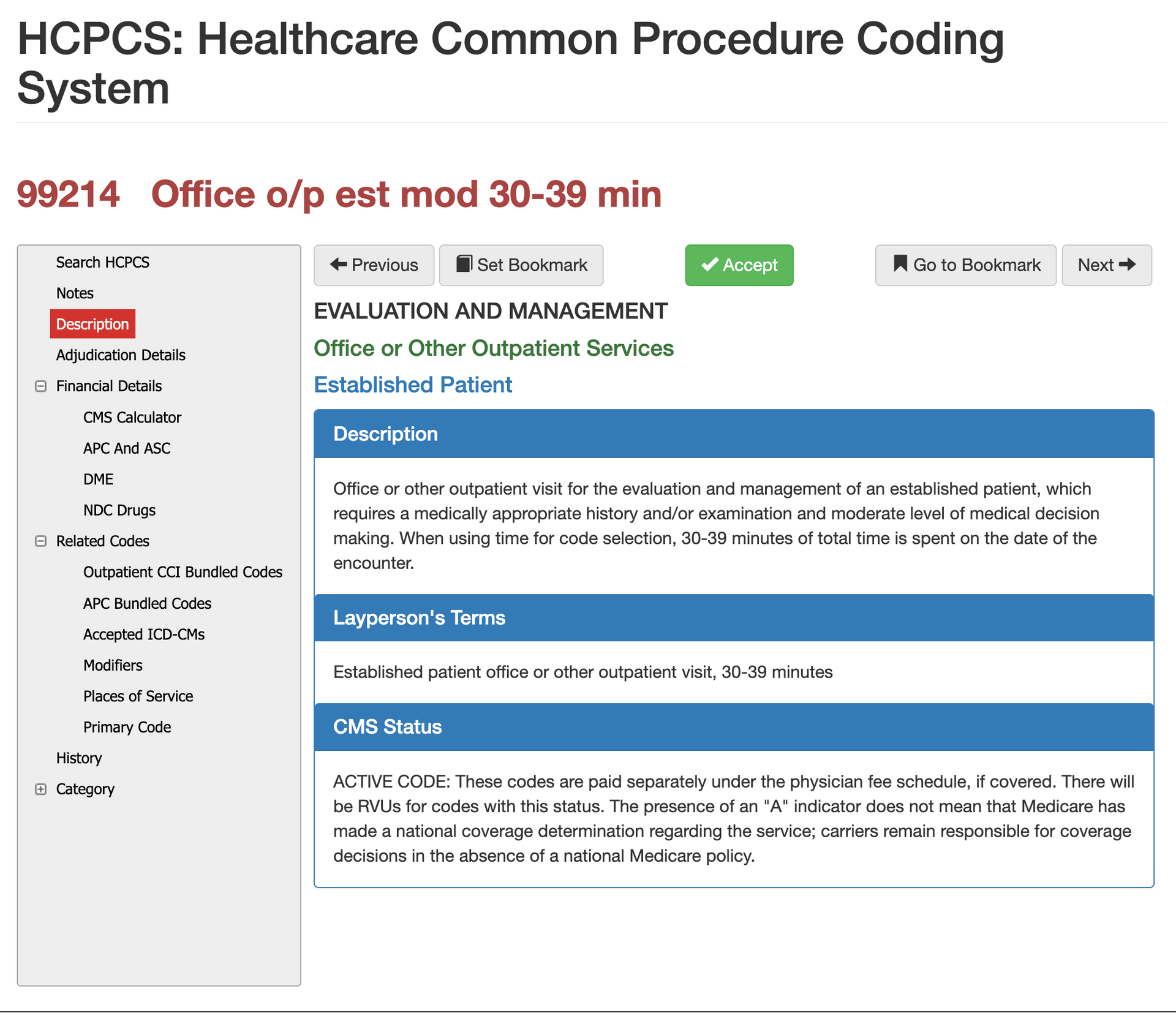
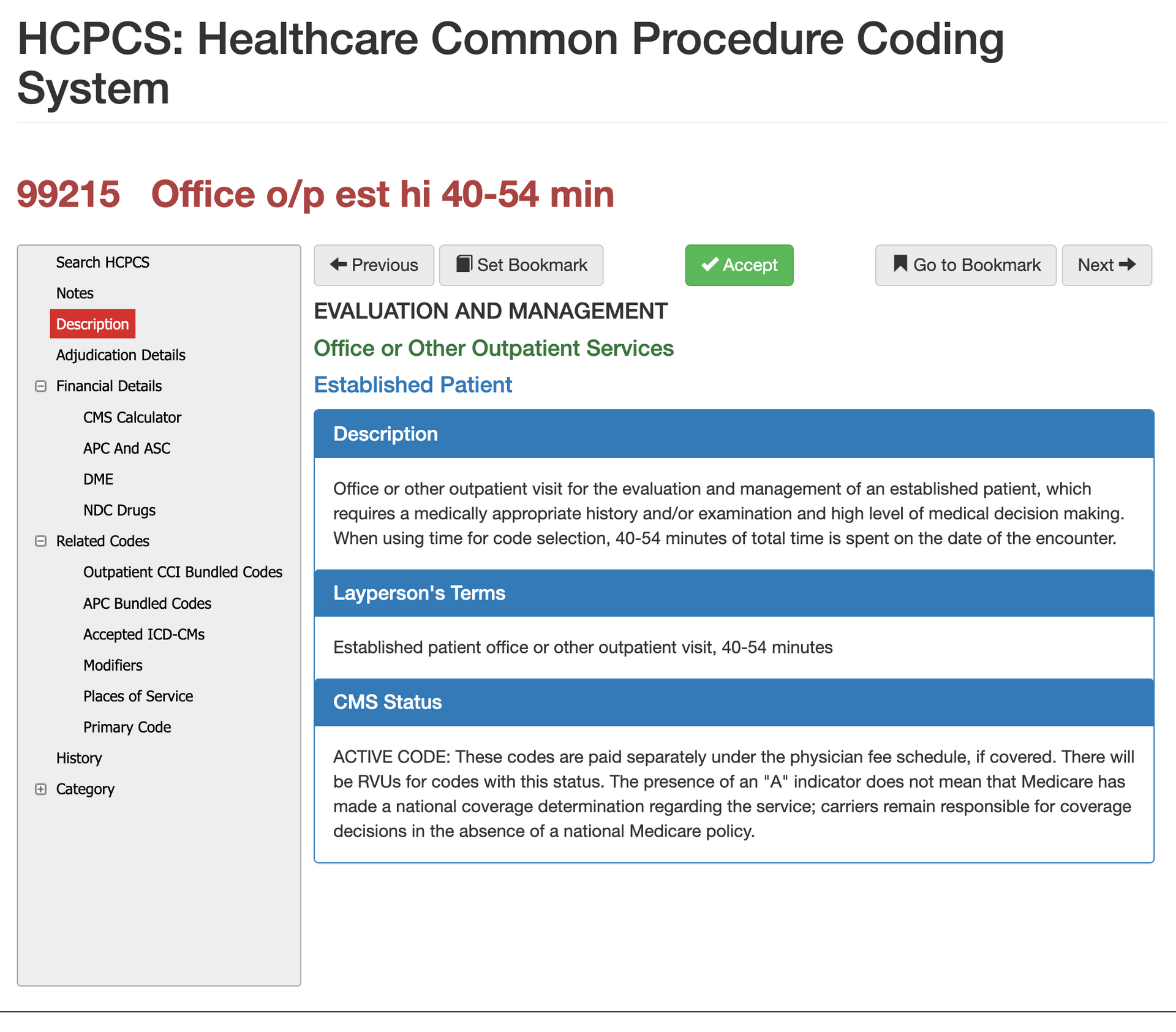
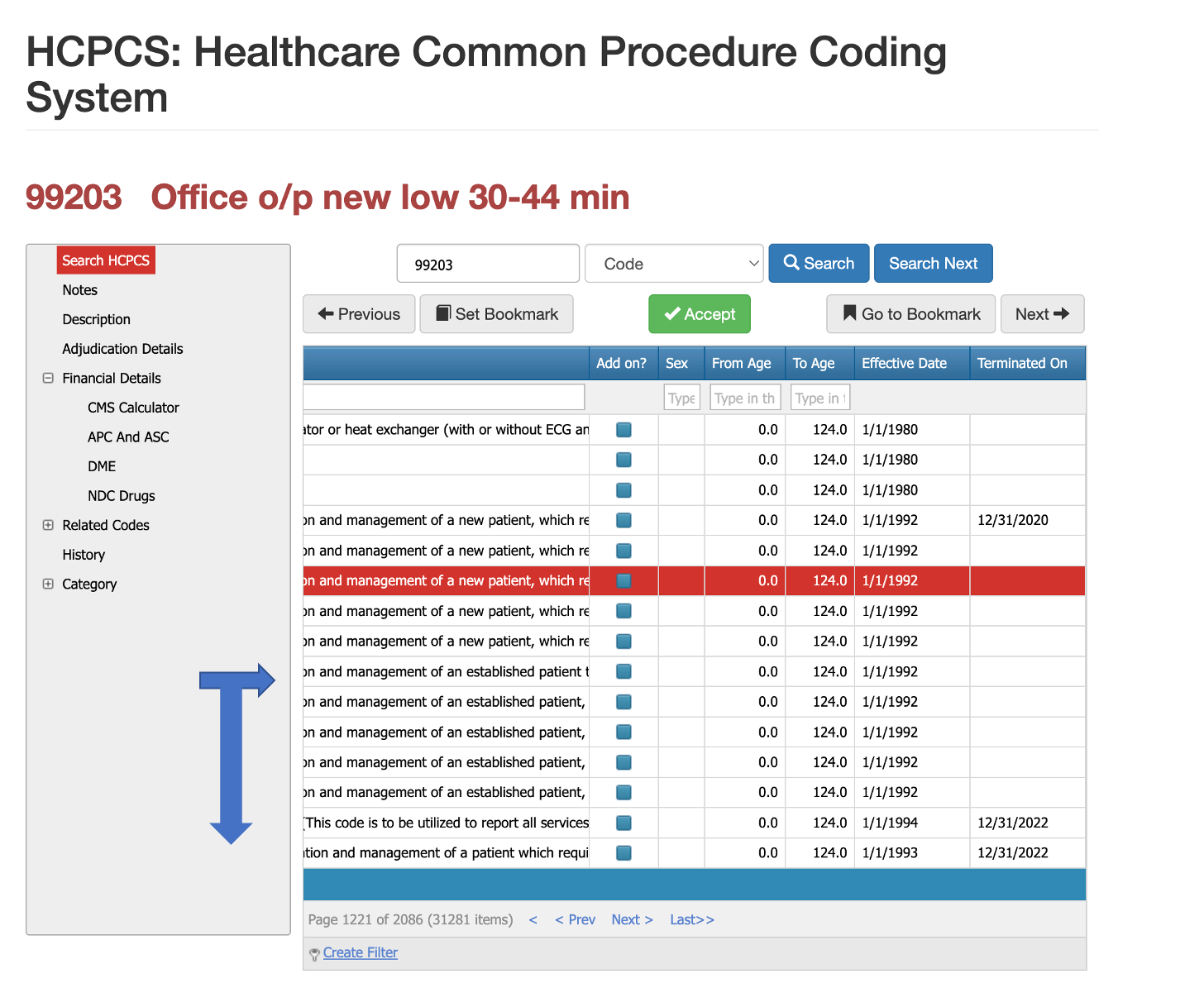
Comparing the 99213 Code with Other Evaluation and Management Codes
Comparing 99212, 99213, 99214, 99215
Conclusions
CPT code 99213 is a follow-up visit in an outpatient setting as an established patient of the provider or provider group. As one of the most commonly used codes in healthcare, it is vital you understand it's modifiers, places of service, time spent with provider (proper usage), bundled codes, and more. We hope you found this blog information and if you'd like to learn more about iVECoder to make your life easier, please click the button below.
Will Schmidt joined PCG Software as their Chief Strategy Officer in November 2022. Prior to PCG, Schmidt lead TNH as their Sr. Vice President to become the 7th largest pharmacy in the nation. He then went on to consult with and serve as Interim CEO or Consultant to over 20 different companies specializing in profit strategies, operational efficiencies, vendor relations and partnerships, and exit strategies, include an international Revenue Cycle Management Company.
Our History and Credibility in Reporting this Information:
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.