CPT 69210 Defined and Usage Explained
Summary:
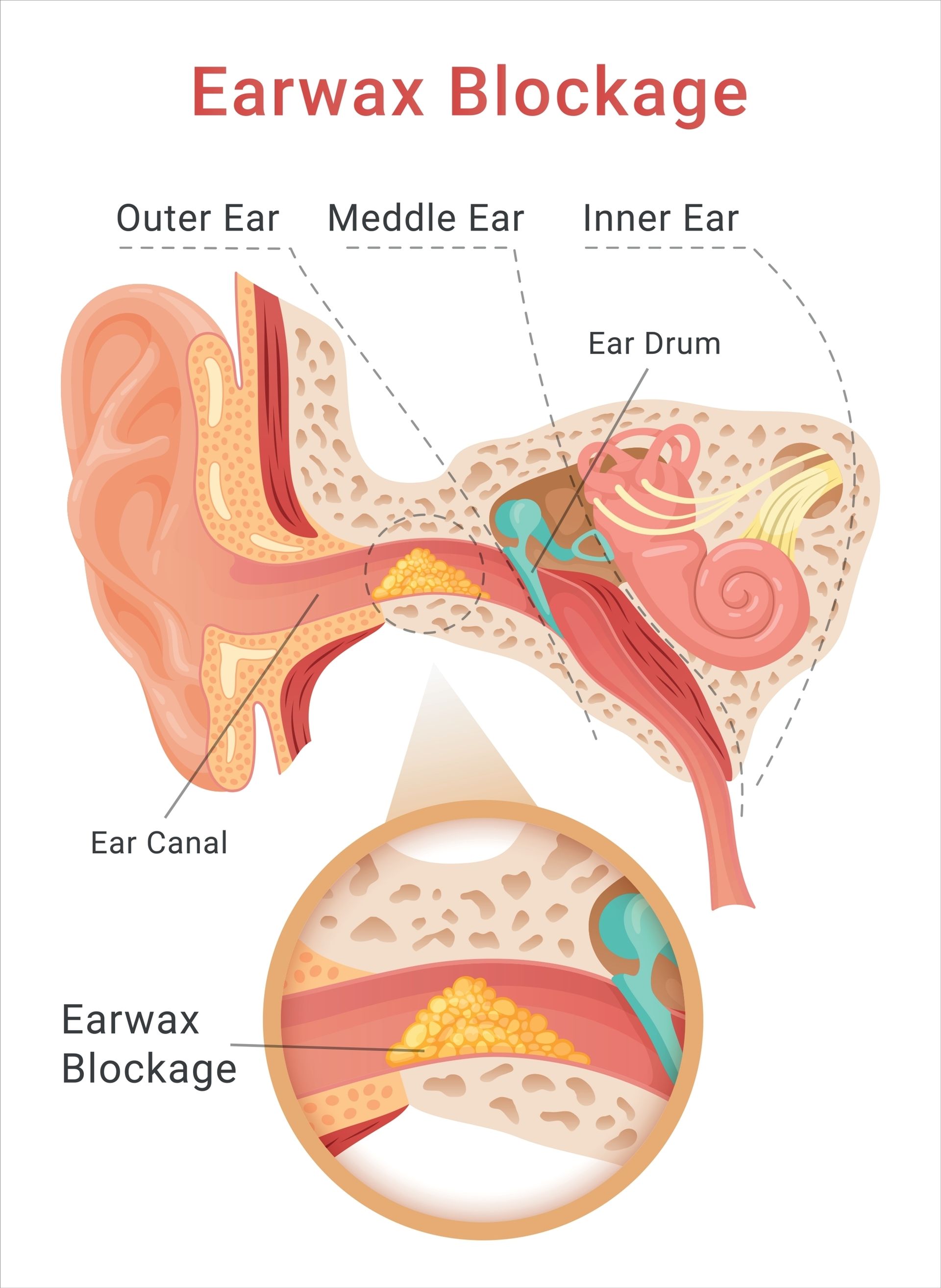
CPT code 69210 is used for the removal of impacted cerumen (earwax) requiring instrumentation, performed unilaterally. This procedure is necessary when earwax is tightly packed, obstructing the ear canal, and causing symptoms such as pain, hearing loss, tinnitus, dizziness, or discomfort. It involves the use of specialized tools like curettes, forceps, or suction devices, distinguishing it from simpler methods like ear irrigation. Documentation must confirm that the cerumen was impacted, describe the tools and techniques used, and explain the medical necessity, such as preparation for audiology testing or relief of symptoms. For bilateral procedures, additional coding modifiers may be required depending on payer guidelines, which should always be reviewed for proper billing and coverage.
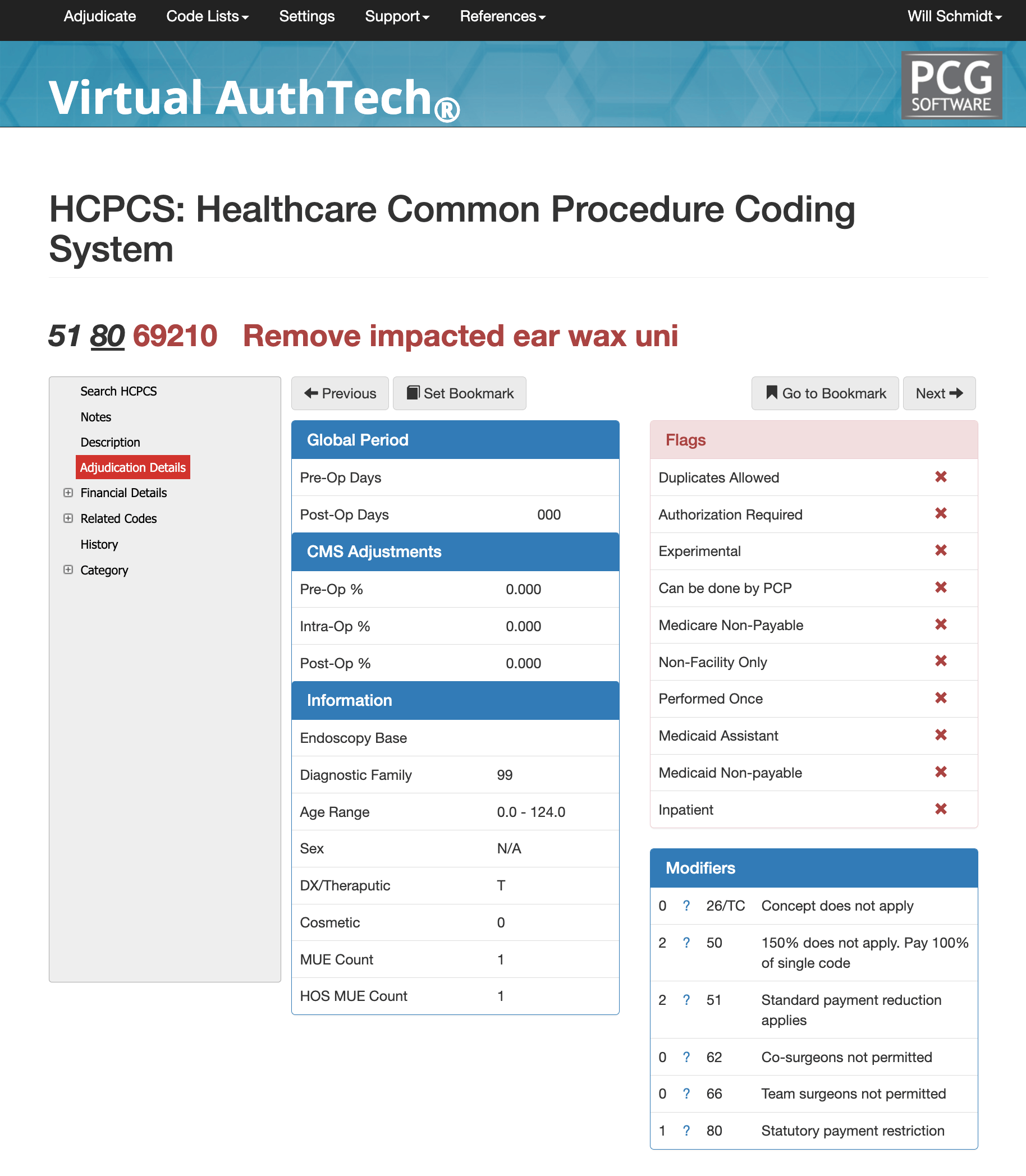
We will dive deeper into this code utilizing our AI medical coding scrubber software Virtual AuthTech which has an AMA license and is updated multiple times every quarter.
AMA Description of CPT 69210
AMA and CMS definition: Removal impacted cerumen requiring instrumentation, unilateral
Layperson: Removal of impacted ear wax
CMS Status: These codes are reimbursed separately under the physician fee schedule, provided they are covered. They will also have assigned RVUs. The "A" indicator does not indicate a national coverage decision by Medicare; local carriers are still responsible for making coverage determinations when no national policy exists.
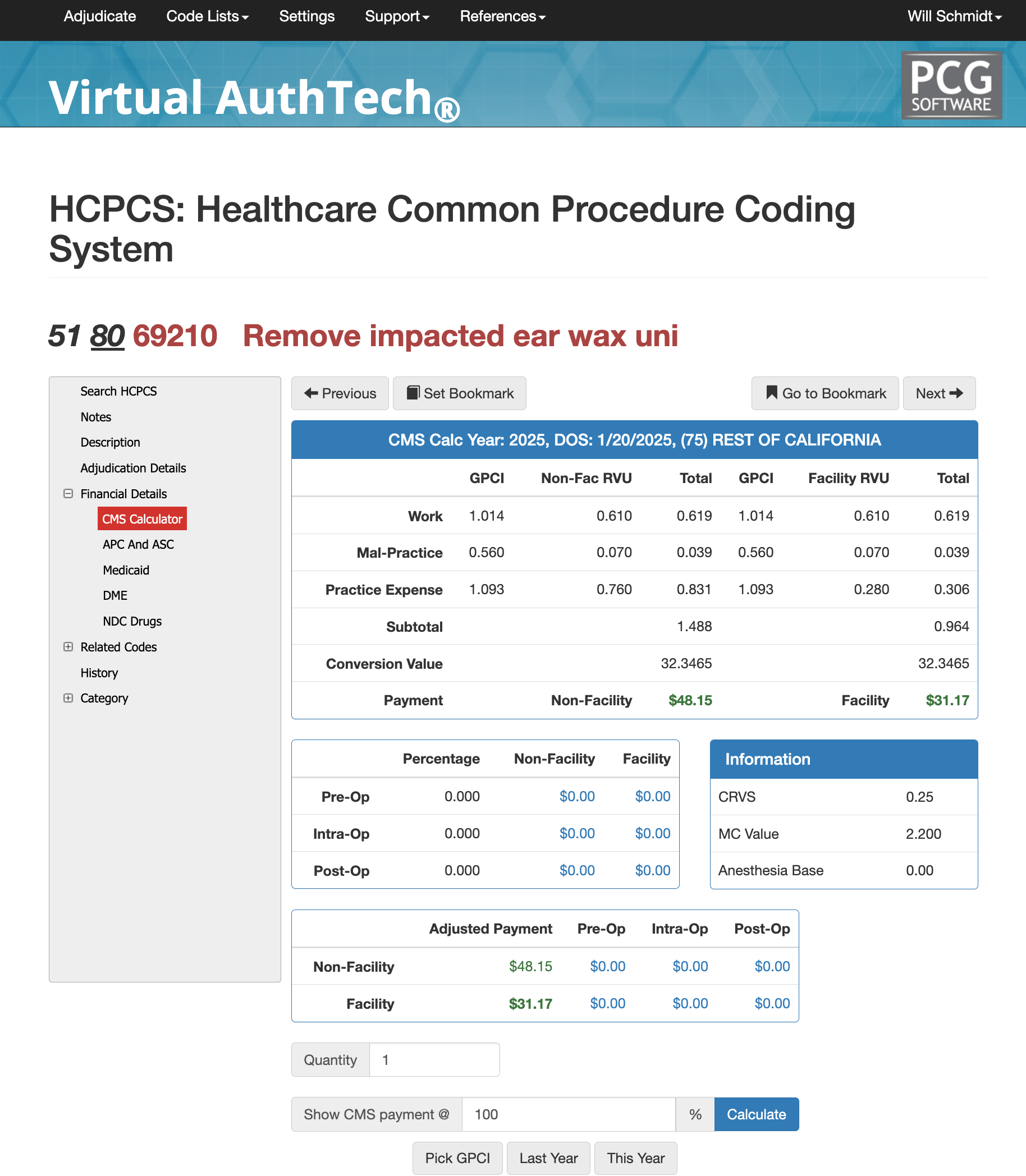
Evaluating Your payment for CPT 20610 against Medicare
Our Virtual AuthTech available to our Virtual Examiner Auditing software clients gives you the ability to search codes and then run analysis on your local GPCI against a percentage of Medicare to evaluate your contracts. In the scenario you see above we see the GPCI for California and the Non-Facility RVU is 0.610 for Works, 0.070 for Mal-Practice, and 0.760 for Practice Expense. Facility RVU is is the same except for Practice Expense which is 0.280. If you use Virtual AuthTech you can input new percentages compared to Medicare to evaluate your plan's contract pricing for providers.
APC, ASC, and Medicaid for CPT Code 69210
APC for 69210
- Group 05733
- Level 3 Minor Procedures
- Payment Weight: 0.66610
- Status Indicator: Q1
- Payment Indicator: 3
- 60%/40% Labor Split: $35.64 / $23.76
- Wage / GEo Adjustment: 54.13 (1.5189)
ASC for 269210
- Payment Indicator: N1
- Description: Remove impacted ear wax uni
- Payment $0.00
- 50% Payment: $0.00
- Wage/GEo Adjustment: $0.00 (1.2645)
- Member Copay @ 20%: $0.00
- Final ASC Payment: $0.00
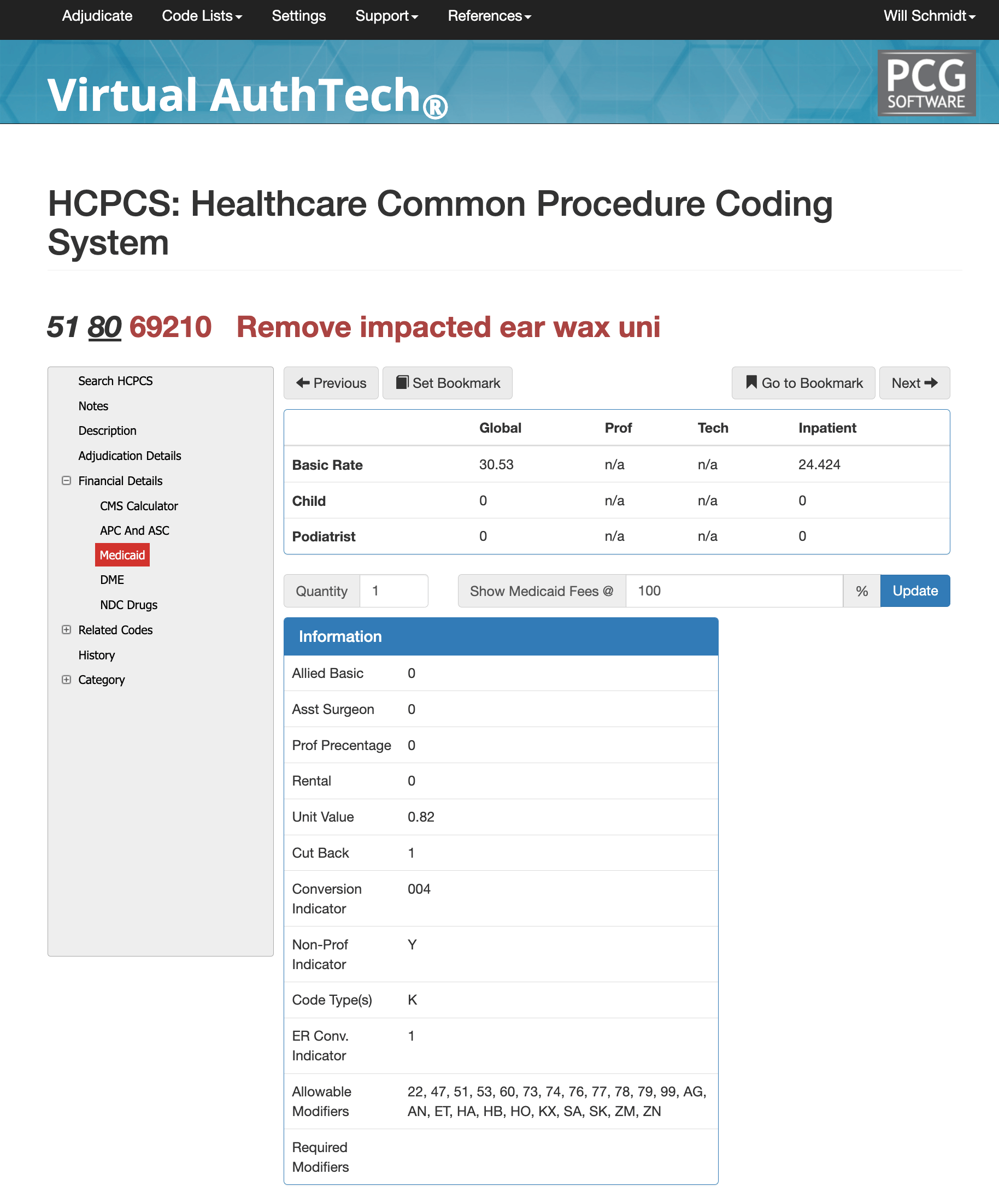
Medicaid, Medi-Cal for CPT 69210
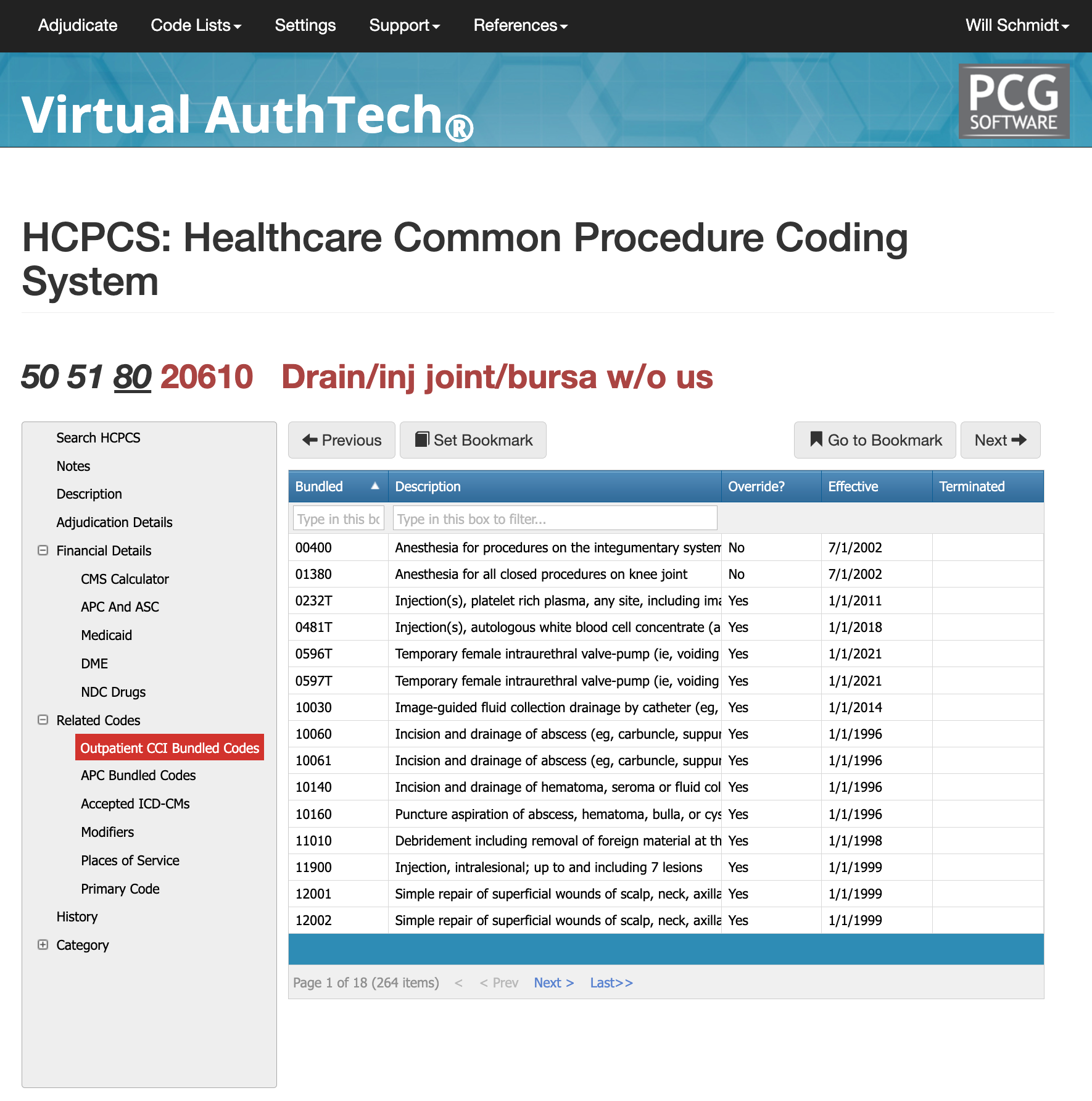
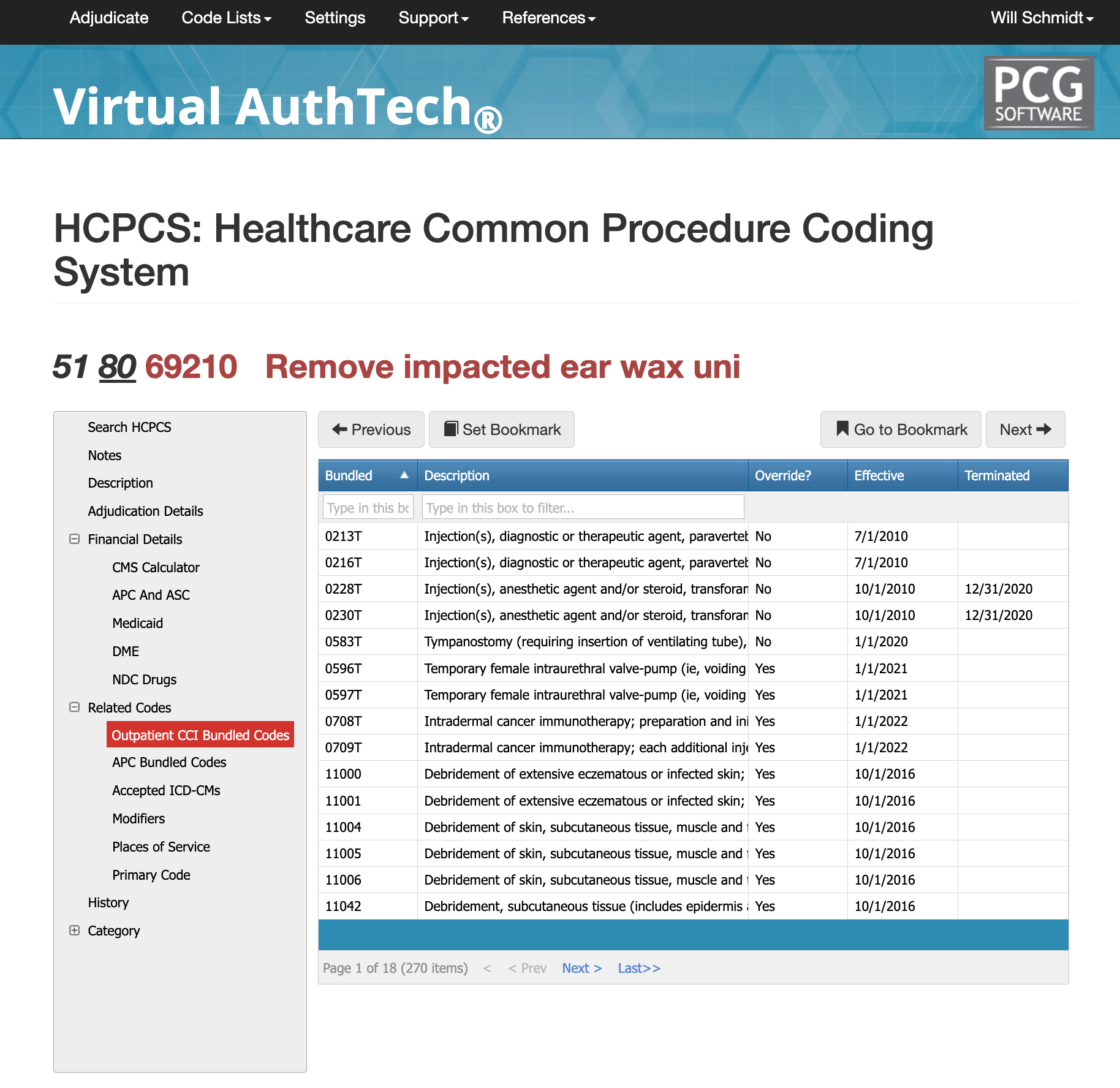
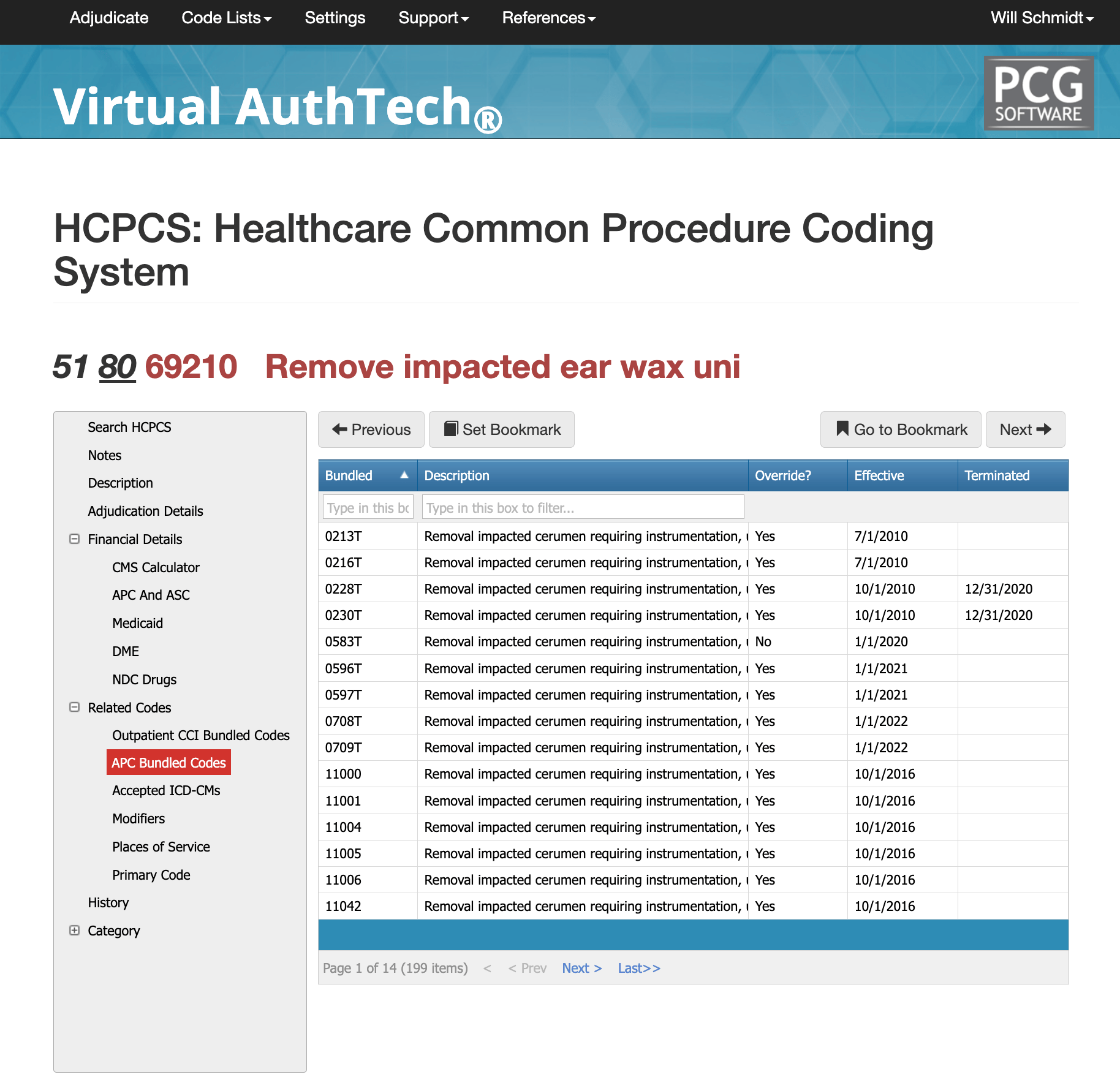
CCI and APC Bundled Codes for 69210
There are over 5,000 possible CCI bundled codes for CPT Code 69210. While normally handled primarily at urgent care, primary care and ear nose and throat (ENT), ear wax removal can be performed by any licensing provider. There over 2800 APC bundled codes as well. To find the most appropriate bundled code you would need to run a mock authorization/adjudication through Virtual AuthTech with your other associated billing codes to find the appropriate bundled code.
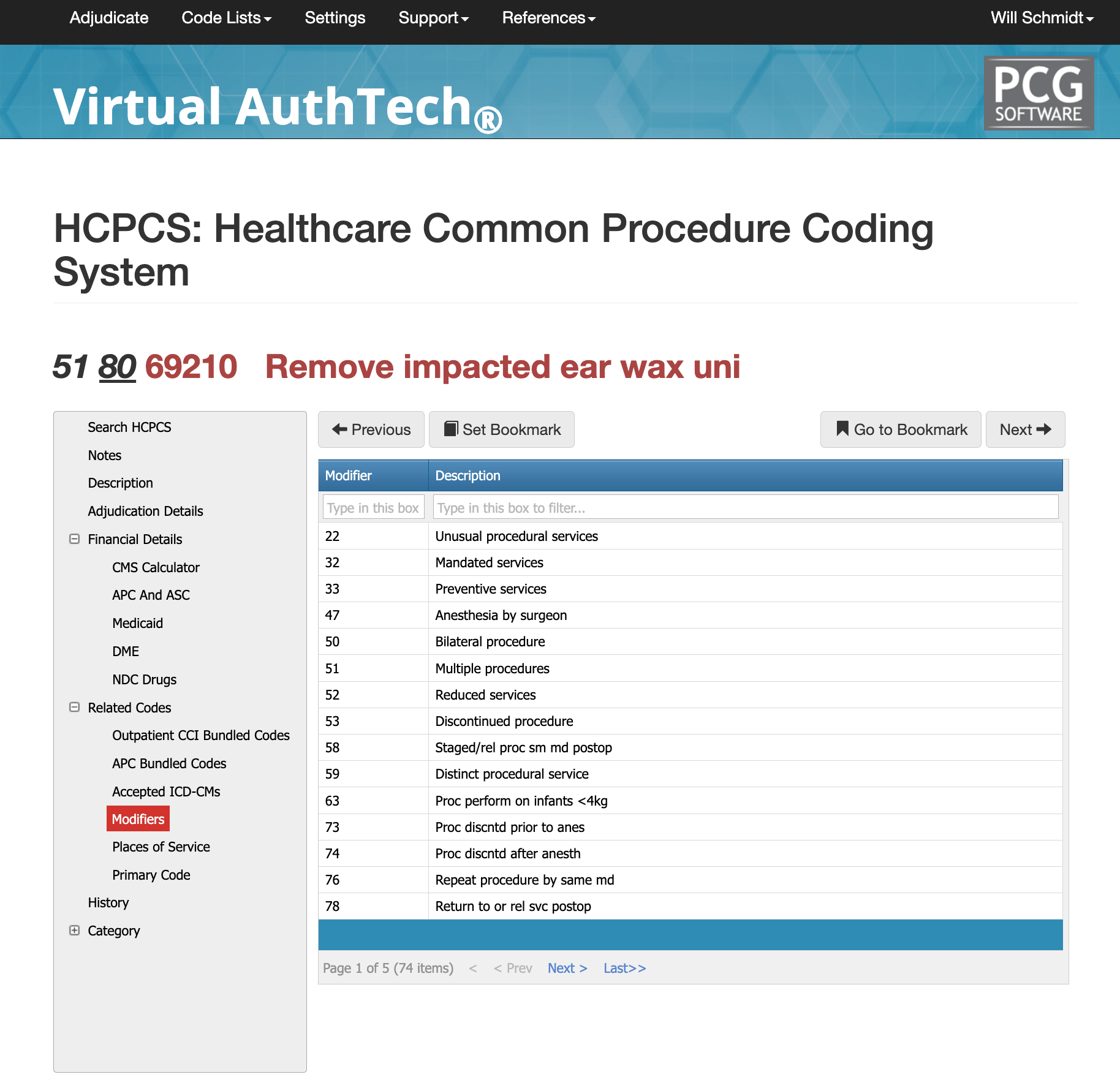
Modifiers for 69210
Here are five common modifiers used with CPT code 69210 and their purposes:
Modifier -50 (Bilateral Procedure):
- Used when the impacted cerumen is removed from both ears during the same session.
- Ensures proper billing for procedures performed on both sides, as CPT code 69210 is inherently unilateral.
Modifier -25 (Significant, Separately Identifiable Evaluation and Management Service):
- Applied when a provider performs a distinct evaluation and management (E/M) service in addition to cerumen removal.
- Demonstrates that the E/M service was necessary and unrelated to the procedure.
Modifier -RT (Right Side):
- Indicates that the procedure was performed on the right ear only.
- Provides clarity for payers when billing for unilateral procedures.
Modifier -LT (Left Side):
- Indicates that the procedure was performed on the left ear only.
- Similarly used to specify unilateral procedures for accurate documentation and billing.
Modifier -59 (Distinct Procedural Service):
- Used when cerumen removal is performed as a separate and distinct procedure from other services provided during the same session.
- Justifies the independent necessity of the procedure to avoid denials for bundling.
These modifiers ensure proper documentation and reimbursement while clarifying the specifics of the procedure performed. Always check payer-specific guidelines, as some modifiers may require additional documentation for approval.
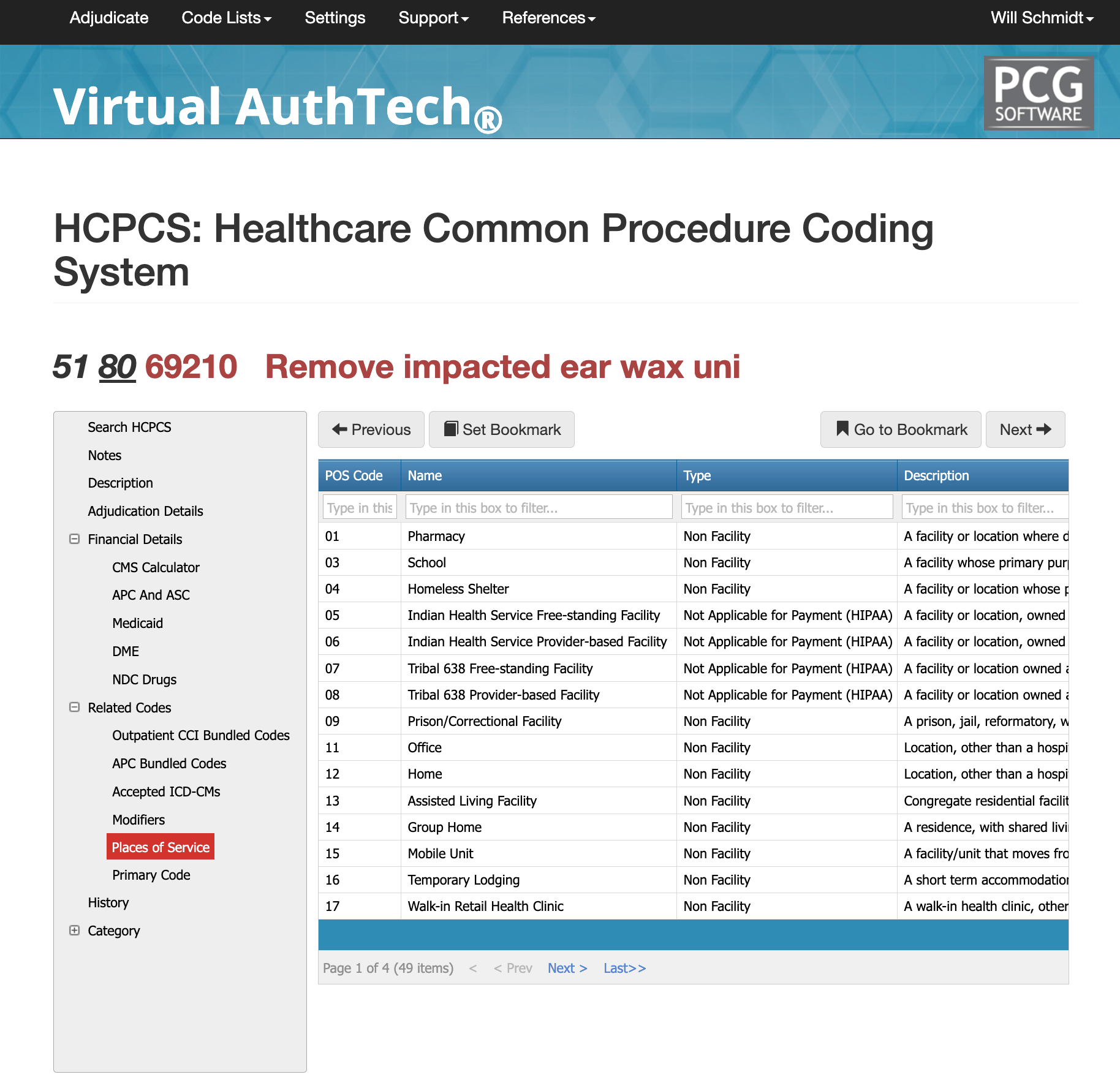
Places of Service for 69210
CPT code 69210 is most commonly approved in settings where impacted cerumen removal is medically necessary and properly documented. These include office visits (POS 11), the most typical setting for routine evaluations or symptom management; outpatient hospitals (POS 22), where the procedure may be part of broader diagnostic services or specialist consultations; and ambulatory surgery centers (POS 24), particularly if specialized equipment or concurrent procedures are involved. It is also frequently performed at urgent care facilities (POS 20) for patients experiencing acute symptoms like pain or hearing loss and in skilled nursing facilities (POS 31) for elderly residents requiring care for discomfort or complications due to impacted earwax. Each setting aligns with payer guidelines when the procedure is justified by symptoms, medical necessity, and proper documentation.
Need more help with CPT Code 69210?
Informative blogs and articles about 69210 are helpful, but an AI code scrubber could save your thousands of hours researching and auditing. Visit our AI claims auditor engine (click for payers), or visit our iVECoder page if you are a clinic.
Our History and Credibility in Reporting this Information:
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.