CPT Code 51703 explained
Summary:
Learn about CPT Code 51703 involving a complicated insertion of bladder tube. Not to be confused with 51701 and 51702 which are temporary insertions of bladder tubes. We'll give definitions, status updates, and visuals to help you submit that next claim or review the claim with more confidence.
Guidelines for 51701 and 51702
Temporary insertions of catheters into the bladder (51701 and 51702). They should only be reported if performed independently. Do not report 51701-51702 when the catheter is an inclusive component of another procedure. CPT 51701 and 51702 are paid separately under the physician fee schedule, if covered. There will be RVUs for codes with this status. The presence of an "A" indicator does not mean that Medicare has made a national coverage determination regarding the service; carriers remain responsible for coverage decisions in the absence of a national Medicare policy.
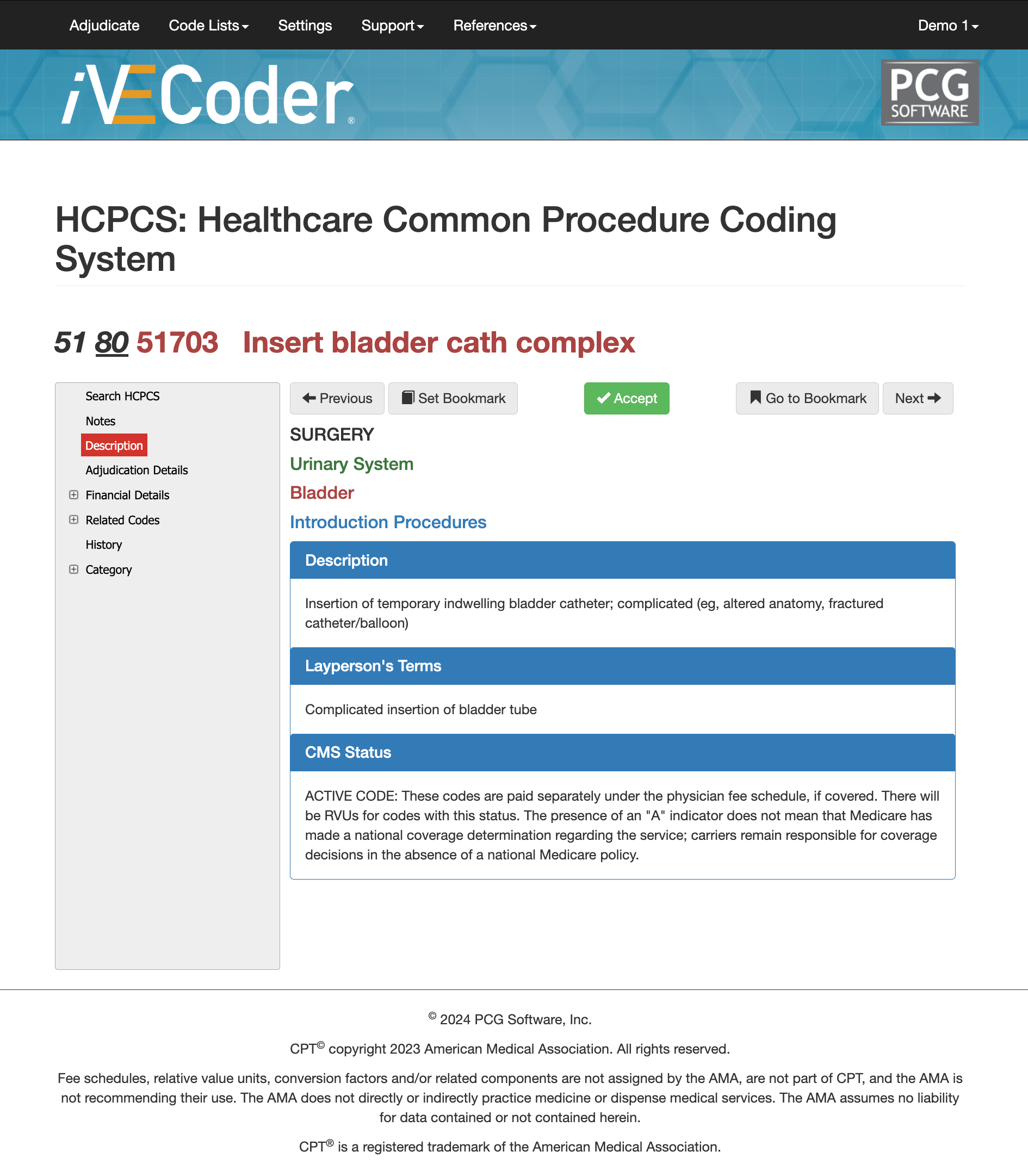
Guidelines for 51703
CPT Code 51703 is a complicated insertion of the bladder tube (layperson definition). The full CMS and AMA description is "Insertion of temporary indwelling bladder catheter; complicated (eg, altered anatomy, fractured catheter/balloon)." These codes are paid separately under the physician fee schedule, if covered. There will be RVUs for codes with this status. The presence of an "A" indicator does not mean that Medicare has made a national coverage determination regarding the service; carriers remain responsible for coverage decisions in the absence of a national Medicare policy.
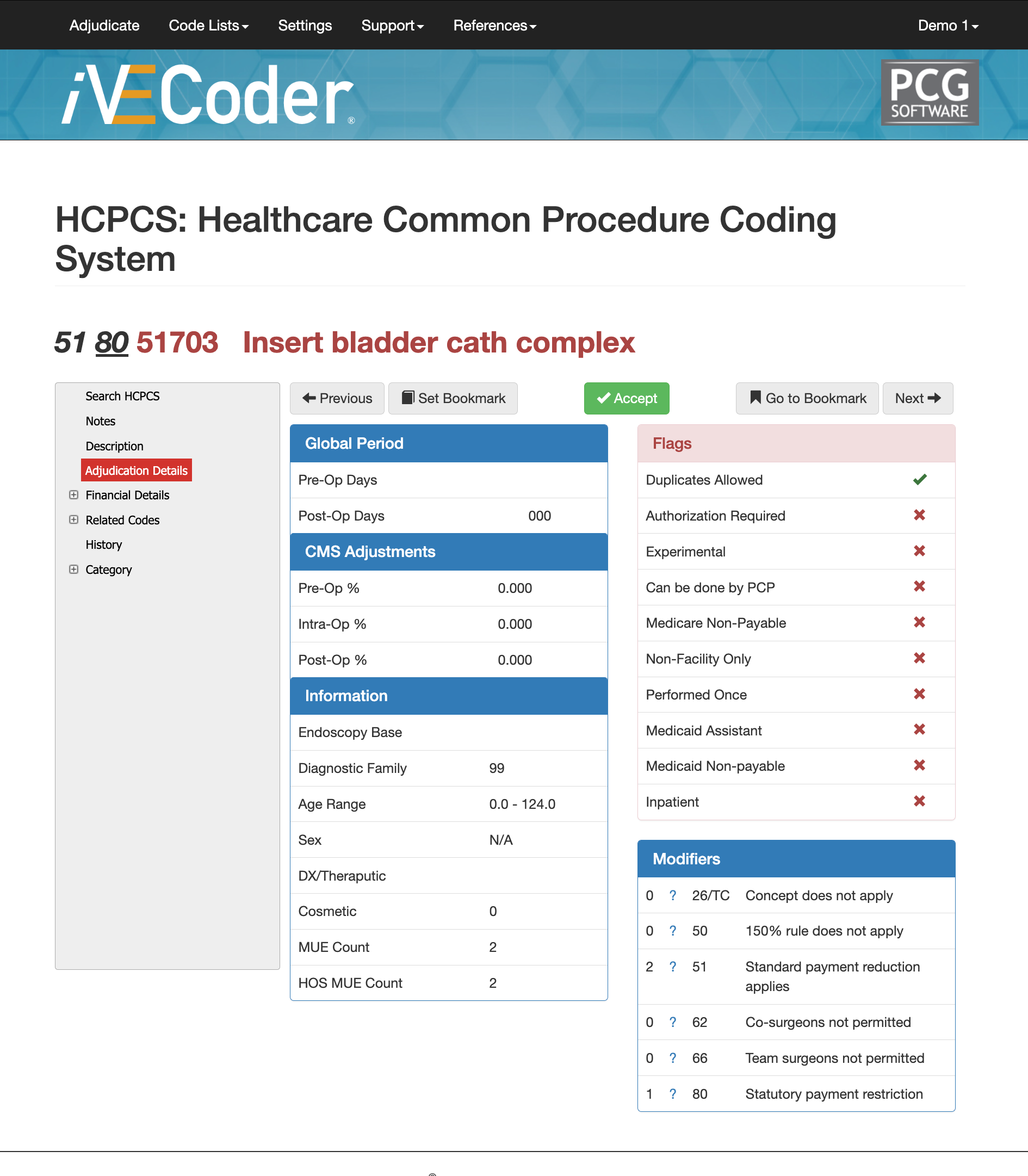
Adjudication Details of CPT Code 51703
01996 cpt code is part of the diagnostic family 99, has no age range, an MUE count of 2, and HOS MUE Count of 2.
Potential Flags for CPT Code 51703
While duplicates are sometimes allowed under specific circumstances it will be based on the physician/payer contract.
51703 cpt code should never be experimental, cannot be done by PCP or a medical assistant, but it can be performed more than once.
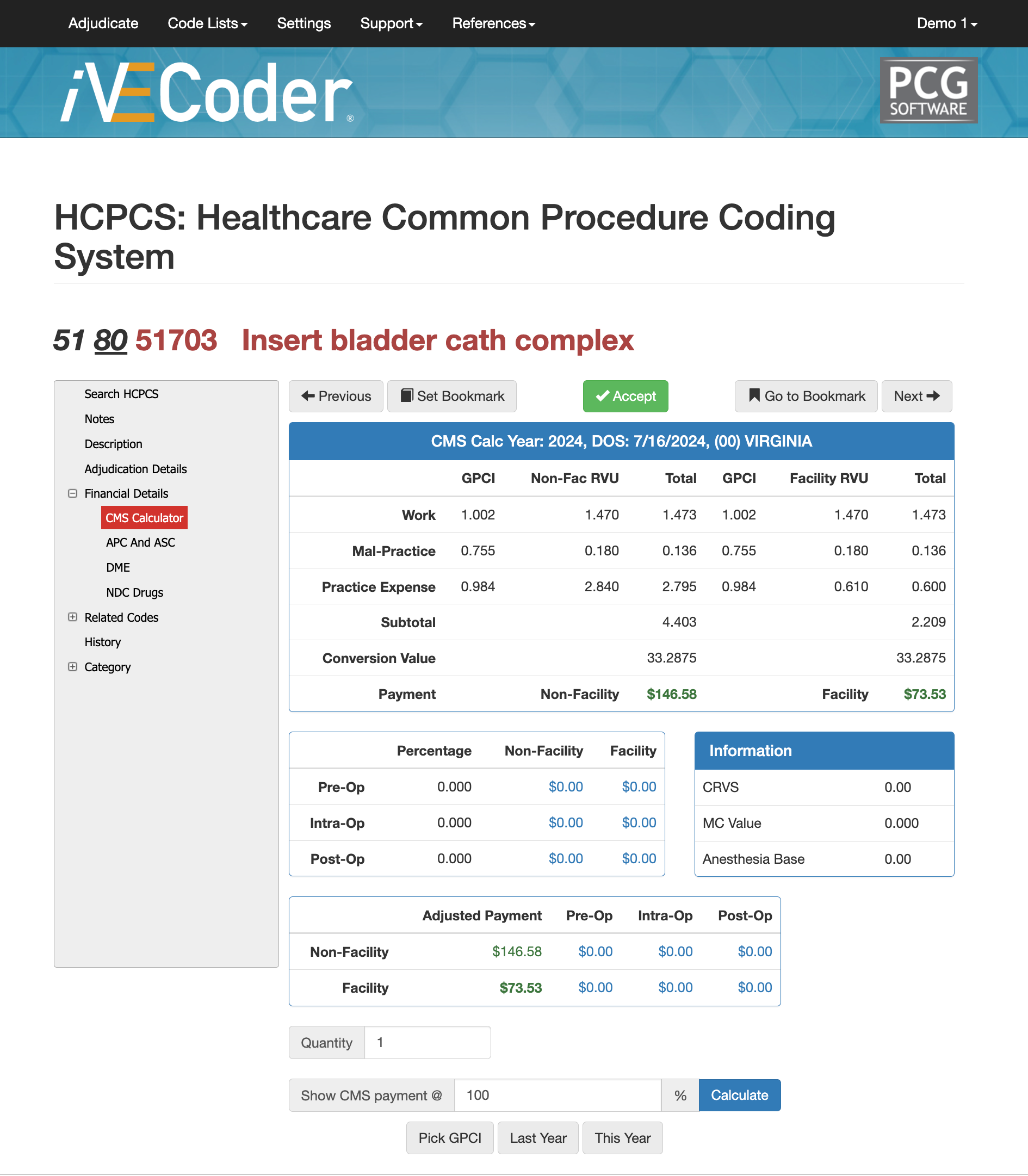
Financial Details of CPT Code 51703
Based on your GPCI you non-facility and facility rates will differ. Using an AI scrubber like iVECoder can help you research the right reimbursement rate your clinic should be getting as well as identify the rate payers should consider when negotiating and setting fees.
By adjusting the "show CMS payment @" in our scrubber, you find different fee amounts and enable both the provider and the payer to establish a fair and yet profitable fee rate for cpt code 51703 and any other medical code and service the provider services.
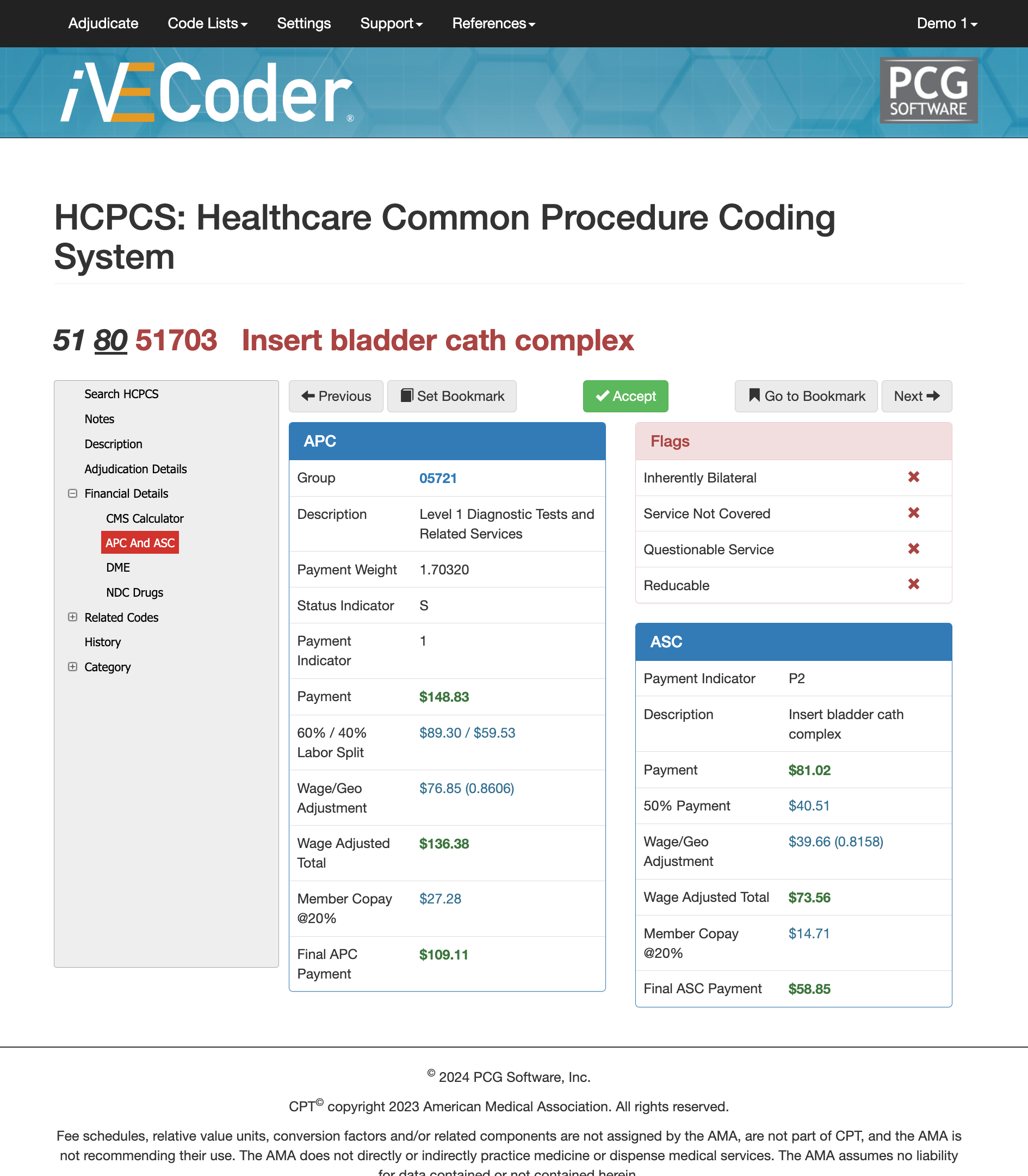
APC and ASC for CPT Code 51703
CPT Code 51703 has an APC group of "05721" and is a level 1 diagnostic tests and related services. The payment weight is set at 1.70320, with status indicate "S" and payment indicator of "1." In our image to the right once you set your GPCI you'll see the 60/40 labor split, wage/GEO adjustments, wage adjusted totals, and approximate member copy amounts.
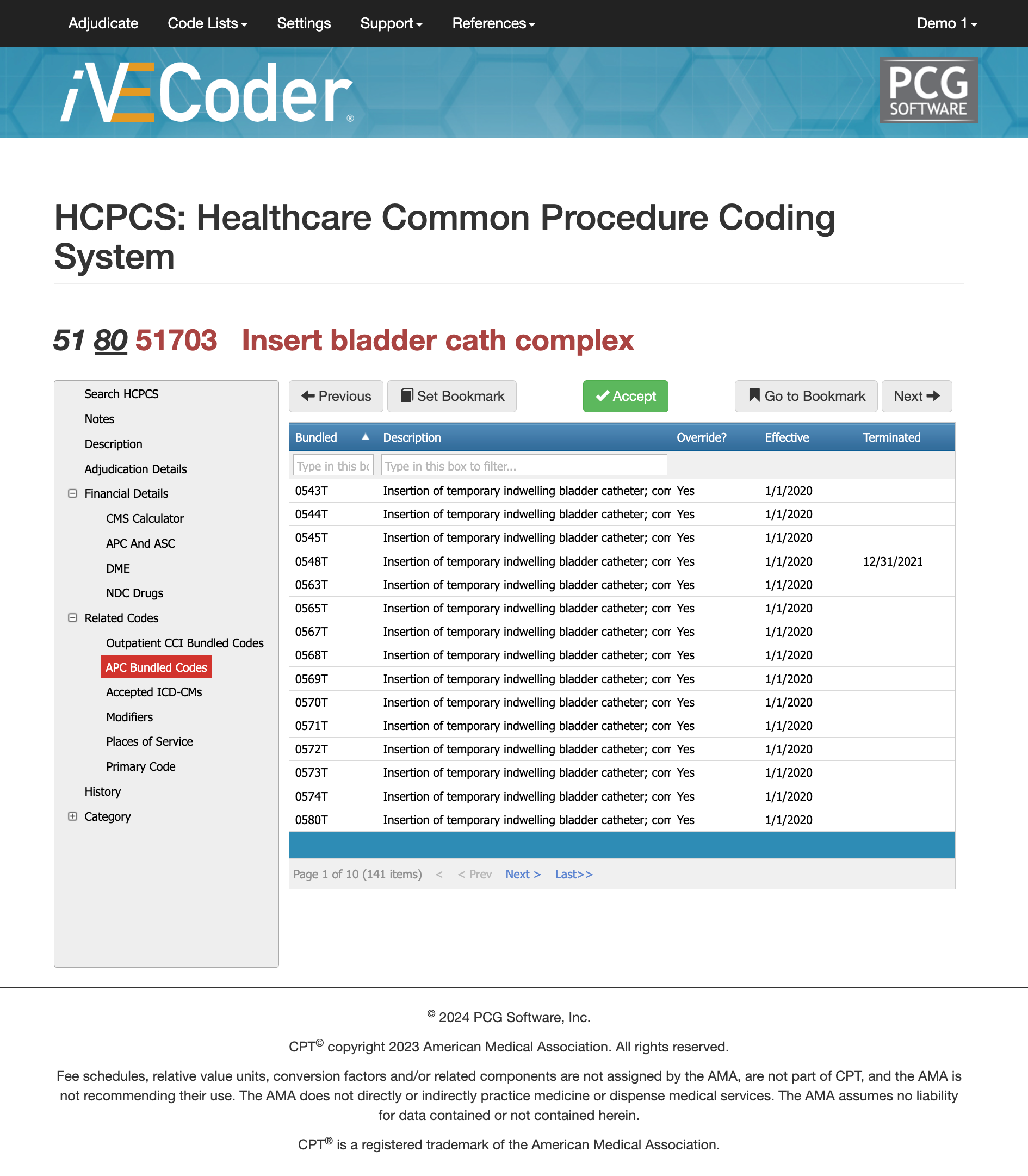
APC Bundled Codes of 51703
What is an APC Bundled Code?
In medical billing, an APC (Ambulatory Payment Classification) bundled code refers to a classification system used by the Centers for Medicare & Medicaid Services (CMS) to determine payment rates for outpatient services provided to Medicare beneficiaries. APCs are part of the Outpatient Prospective Payment System (OPPS), which is designed to standardize payments and control costs for outpatient care.
How many apply to 51703?
There are 141 possible APC Bundled codes that could apply to cpt code 51703. Unbunlding the code can result in a denial, or invalid approval and payment leading to a later audit with financial loss. It is important that you use a scrubber, examine the medical notes and history and use the appropriate APC bundled code if applicable.
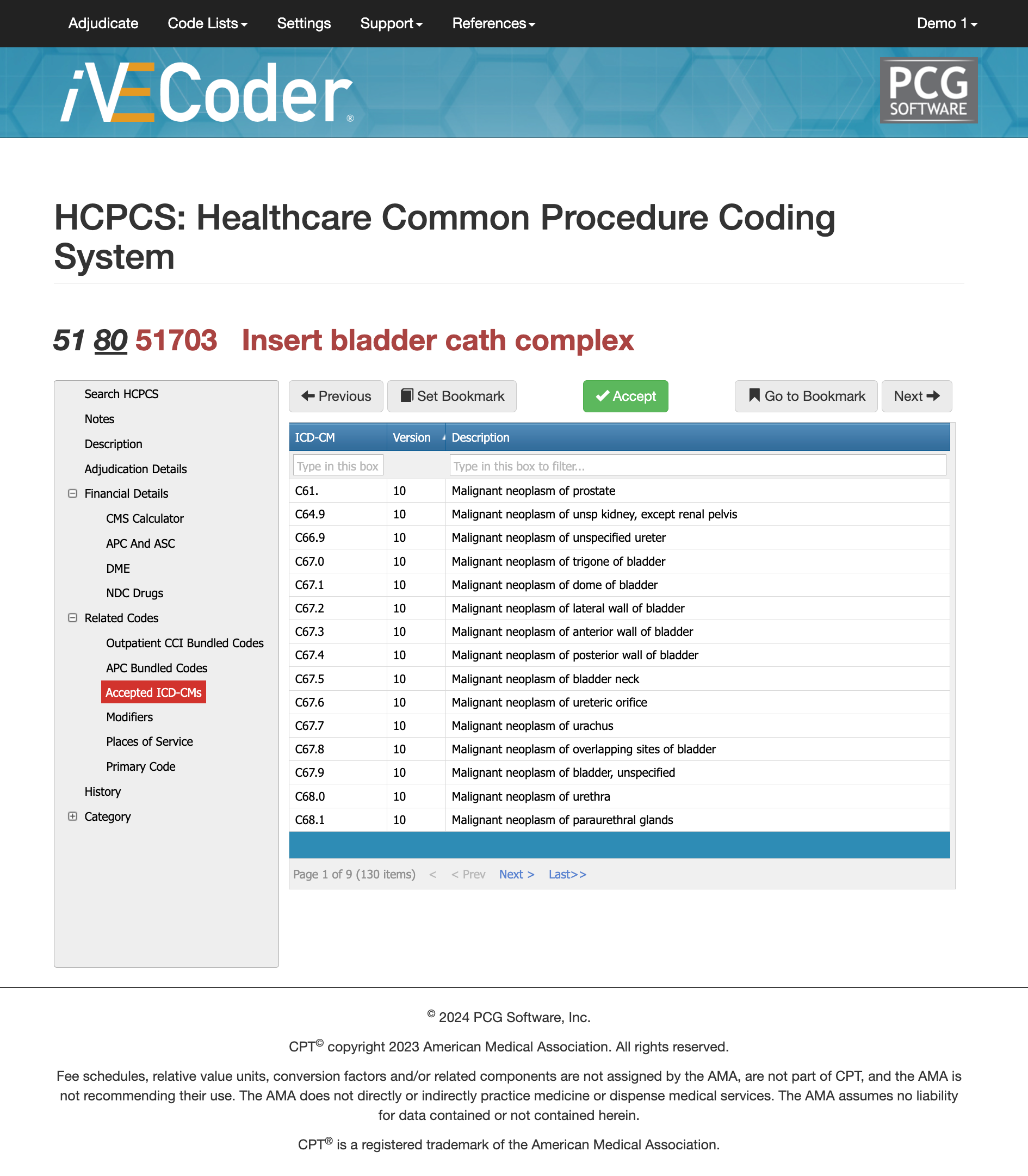
Accepted ICDs for CPT Code 51703
There are over 130 ICDs right now that could apply to the billing of cpt code 51703. Be especially careful when citing "Malignant Neoplasm of" because there is prostate, kidney, ureter, trigone of bladder, dome of bladder, and many other different ICDs that could apply. While submitting incorrectly a payer can still pay you for the service only later on coming back for an audit to clean their encounter data and you're left with a denial requesting for correct resubmission of your diagnosis. You would be faced with at least $40 in administrative fees alone for the appeal.
Using our iVECoder on it's home page (adjudication page), you search for the correct ICD based on the physician's medical notes and apply to your mock adjudication to ensure that you ICD is correct and that follows CMS and AMA guidelines.
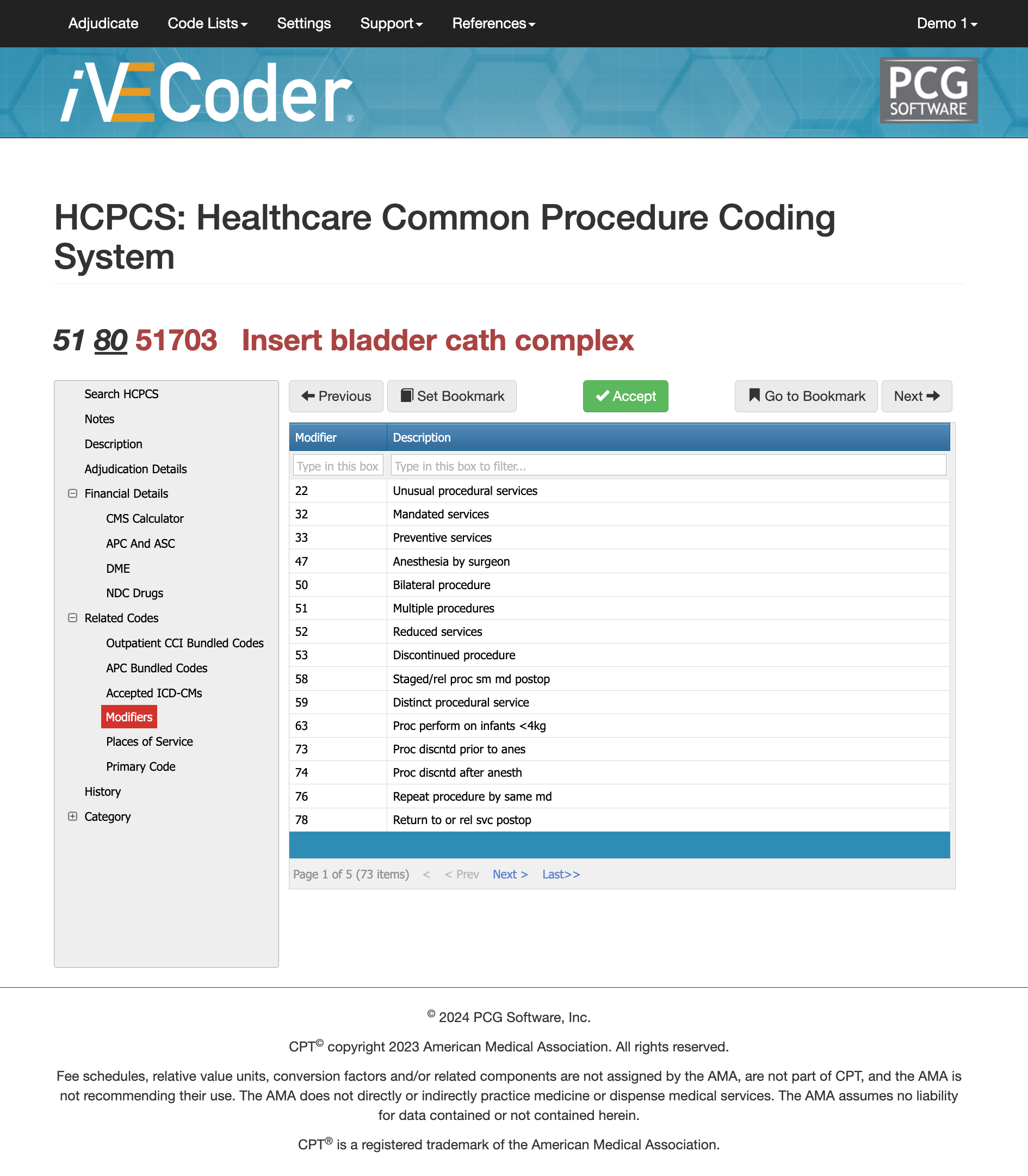
Modifier Usage for CPT Code 51703
Modifier -59 (Distinct Procedural Service):
This modifier indicates that the procedure was distinct or independent from other services performed on the same day. It is used when procedures that are typically bundled together are performed in separate and distinct settings or encounters.
Modifier -25 (Significant, Separately Identifiable Evaluation and Management Service):
Used when a significant and separately identifiable E/M service is performed by the same physician or other qualified health care professional on the same day as the procedure. This means an evaluation and management service was provided above and beyond the other service.
Modifier -51 (Multiple Procedures):
This modifier is used when multiple procedures are performed during the same session. It indicates that multiple services were provided and helps in the correct reimbursement of each service.
Modifier -76 (Repeat Procedure or Service by Same Physician or Other Qualified Health Care Professional):
This modifier is used when the same procedure is performed more than once on the same day by the same provider. It indicates that the procedure was repeated.
Modifier -77 (Repeat Procedure by Another Physician or Other Qualified Health Care Professional):
This modifier is used when the procedure is repeated by a different provider on the same day. It distinguishes the repeat procedure from the original procedure performed by another provider.
Modifier -52 (Reduced Services):
This modifier indicates that a service or procedure was partially reduced or eliminated at the physician’s discretion. It is used when the full service described by the CPT code is not performed.
Using the appropriate modifiers is crucial for ensuring accurate coding and proper reimbursement. By using iVECoder you can run mock authorizations and adjudications with different modifiers to see the likelihood of getting a medical claim approved and learning which modifiers work best with CPT Code 51703.
51703 CPT Code Final Thoughts
CPT Cod 51703 is a very common medical code used by emergency rooms and hospitals every day. It's important to draw the distinction between complicated catheters (51703) and temporary catheters (51701 and 50172). Using an AI medical coding scrubber (iVECoder) or having iVECoder integrated into your EMR/EHR or billing software can quickly help you avoid denials and speed up your entire RCM process and remain compliant with not just 51703 but every possible code in the US healthcare system.
Quick Links:
Will Schmidt joined PCG Software as their Chief Strategy Officer in November 2022. Prior to PCG, Schmidt lead TNH as their Sr. Vice President to become the 7th largest pharmacy in the nation. He then went on to consult with and serve as Interim CEO or Consultant to over 20 different companies specializing in profit strategies, operational efficiencies, vendor relations and partnerships, and exit strategies, include an international Revenue Cycle Management Company.
Our History and Credibility in Reporting this Information:
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.