CPT 20610 Defined and Usage Explained
Summary:
CPT code 20610 refers to procedures involving the aspiration and/or injection of fluid from major joints or bursae, such as the shoulder, hip, knee, or subacromial bursa, without the use of ultrasound guidance. This procedure is often used to treat conditions like joint inflammation or fluid buildup. If imaging guidance (such as ultrasound or fluoroscopy) is used, separate CPT codes may apply. This code is active under the Medicare Physician Fee Schedule and is reimbursed separately if covered, although local Medicare carriers are responsible for making coverage determinations in the absence of a national policy.
AMA Description of CPT 20610
There's always a CMS/AMA definition and a layperson's term, see them here:
Arthrocentesis, aspiration and/or injection, major joint or bursa (eg, shoulder, hip, knee, subacromial bursa); without ultrasound guidance.
Layperson:
- Aspiration and/or injection of fluid from large joint.
- May be coded as 20610 Drain/inj join/burse w/o us (50, 51, 80)
Current CMS Status of CPT 20610
ACTIVE CODE: These codes are reimbursed separately under the physician fee schedule, provided they are covered. They will also have assigned RVUs. The "A" indicator does not indicate a national coverage decision by Medicare; local carriers are still responsible for making coverage determinations when no national policy exists.
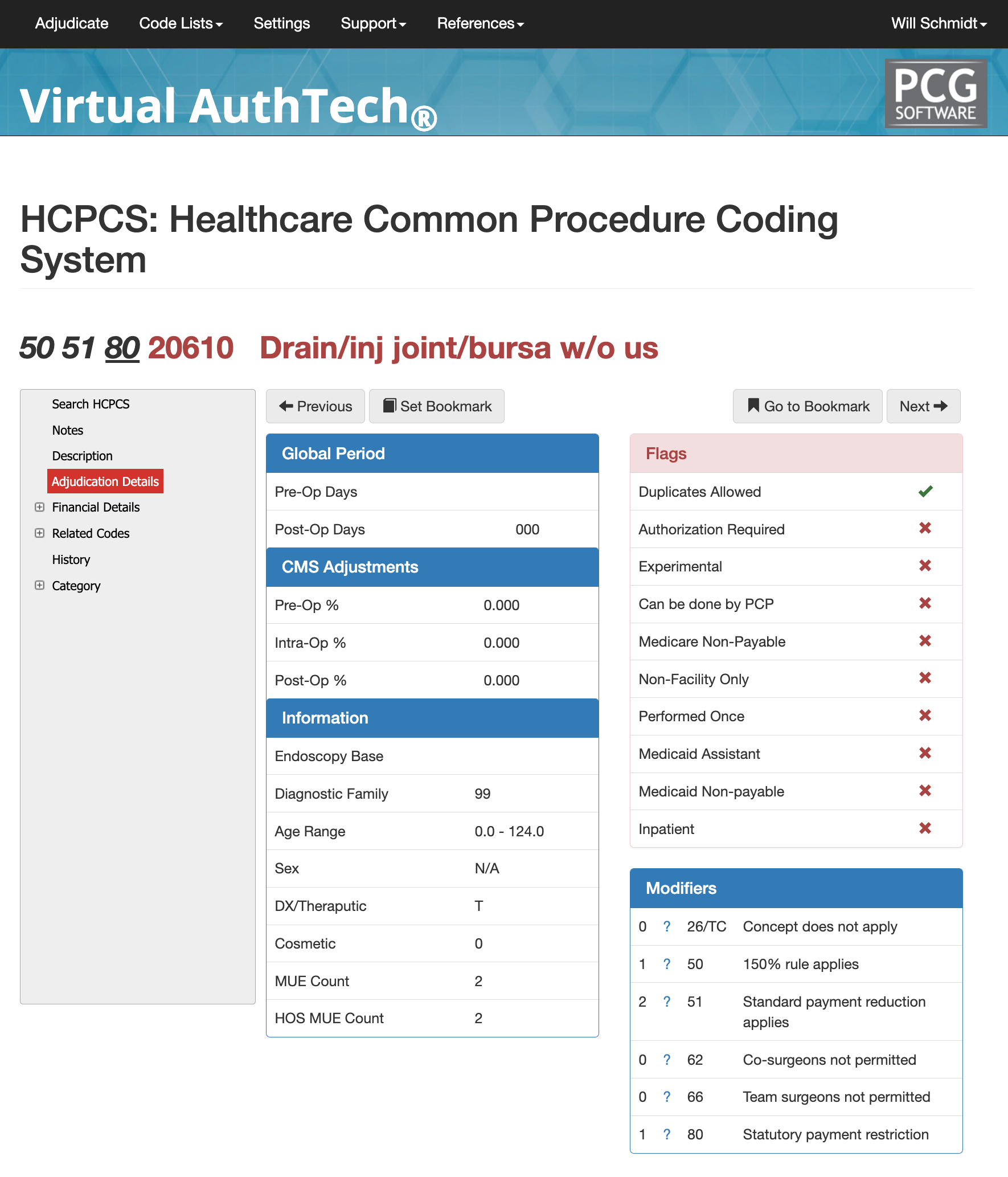
Ajudication Details for CPT Code 20610
- Pre-op Days: n/a
- Post-op Days: 000
- CMS Adjustments:
- Pre-op% 0.000
- Intra-op% is 0.000
- Post-Op% is 0.000
- Information:
- Diagnostic Family 99
- Age Range: 0.0 - 124.0
- Sex: n/a
- DX/Therapeutic: %
- Cosmetic: 0
- MUE Count: 2
- HOS MUE Count: 2
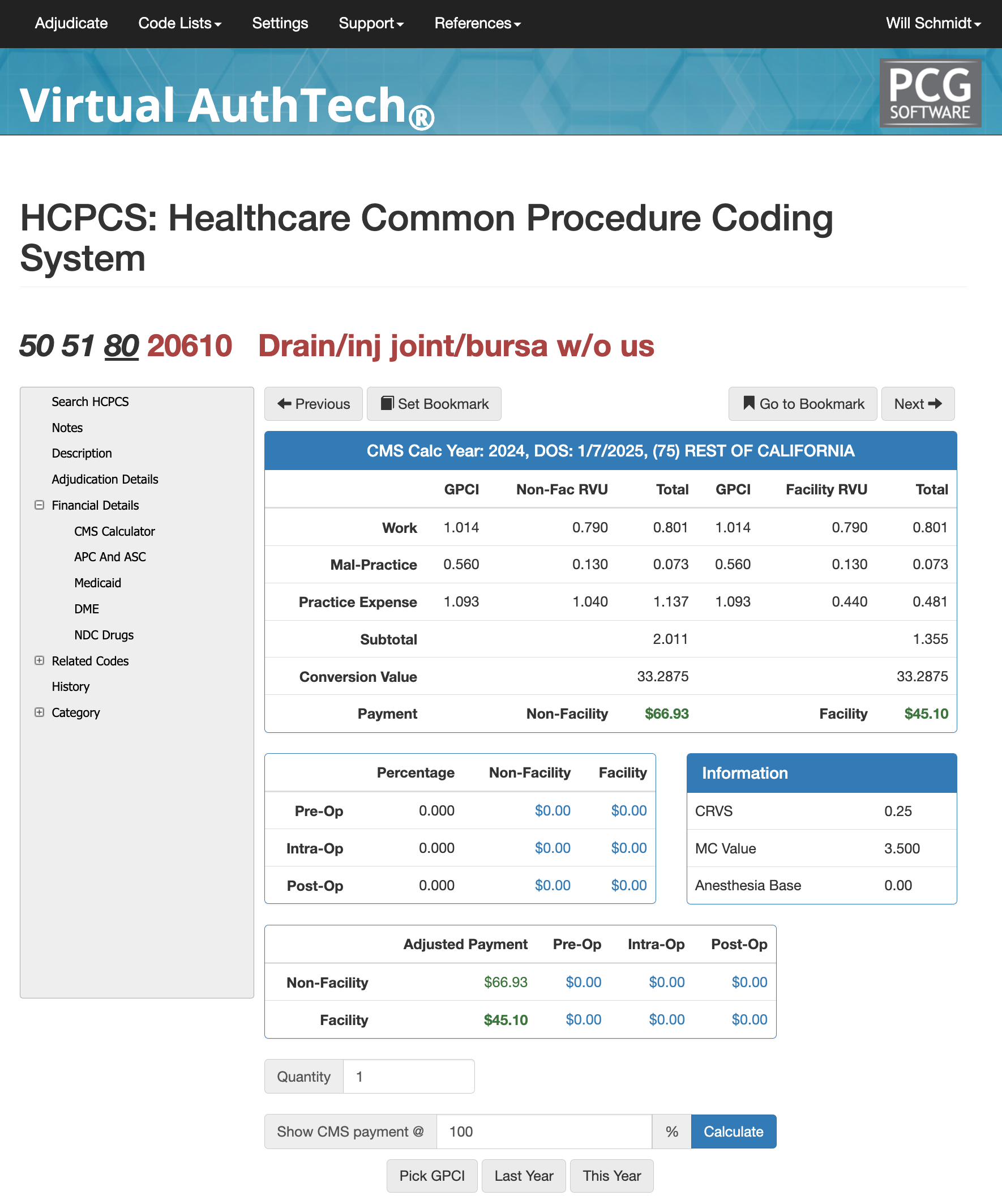
Evaluating Your payment for CPT 20610 against Medicare
Our Virtual AuthTech available to our Virtual Examiner Auditing software clients gives you the ability to search codes and then run analysis on your local GPCI against a percentage of Medicare to evaluate your contracts. In the scenario you see above we see the GPCI for California and the Non-Facility RVU is 0.790 with Facility RVU the same. The Non-Facility payment would be $66.93 and the Facility payment would $45.10 (that's at 100% to CMS payment. By
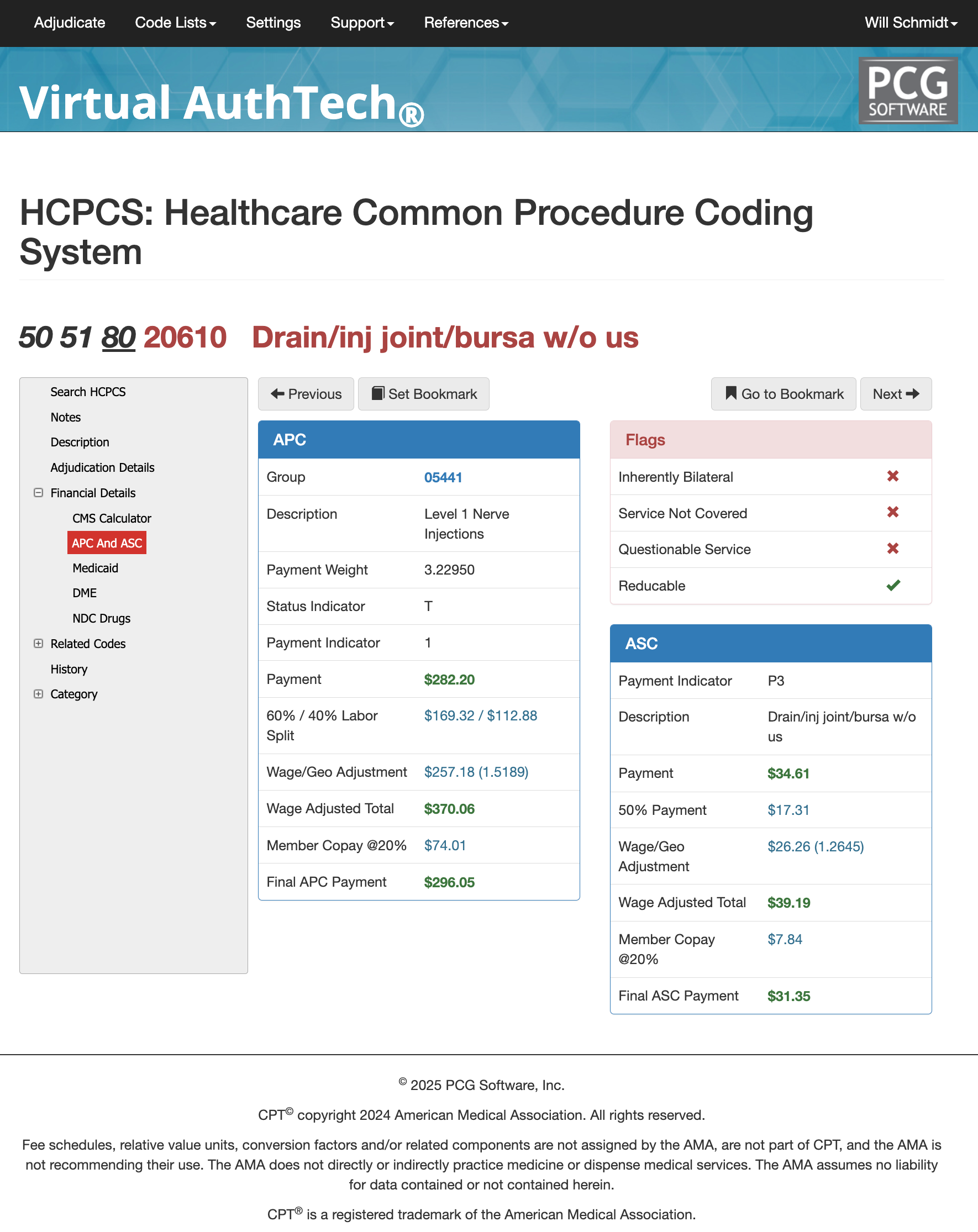
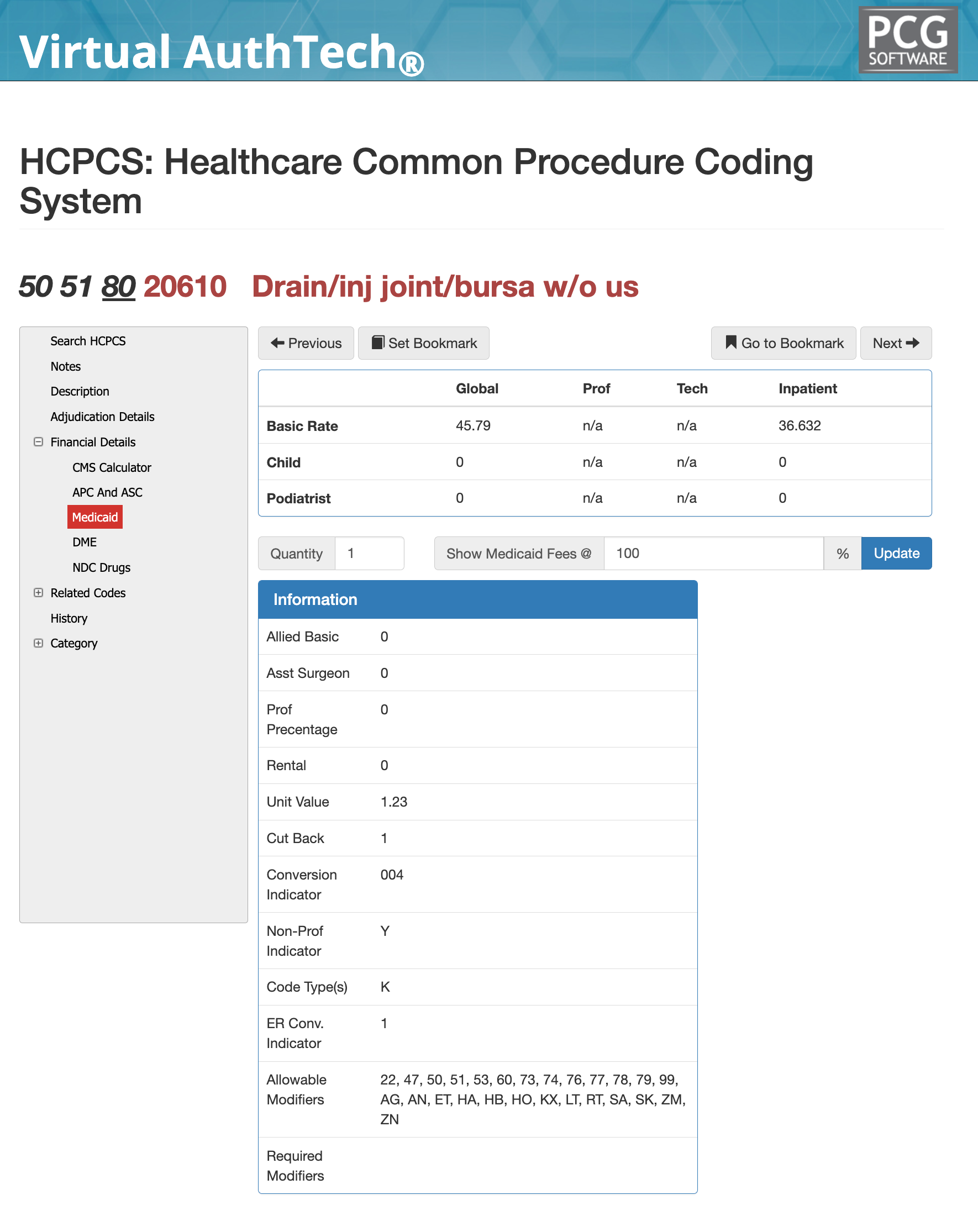
APC, ASC, and Medicaid for CPT Code 20610
The picture below illustrates VA's findings for CPT Code 20610 against APC, ASC, and California Medicaid (Medi-Cal). You would want to set your GPCI and state medicaid settings for your own company location.
APC for 20610
- Group 05441
- Level 1 Nerve Injections
- Payment Weight: 3.22950
- Status Indicator: %
- Payment Indicator: 1
- 60%/40% Labor Split: $169.32 / $112.88
- Wage / GEo Adjustment: $257.18
ASC for 20610
- Payment Indicator: P3
- Description: Drain/inj joint/bursa w/o us
- Payment $34.61
- Wage/Geo Adjustment $26.26 (1.2645)
- Wage Adjusted Total $39.19
- Member Copay @ 20%: $7.84
- Final ASC Payment: $31.35
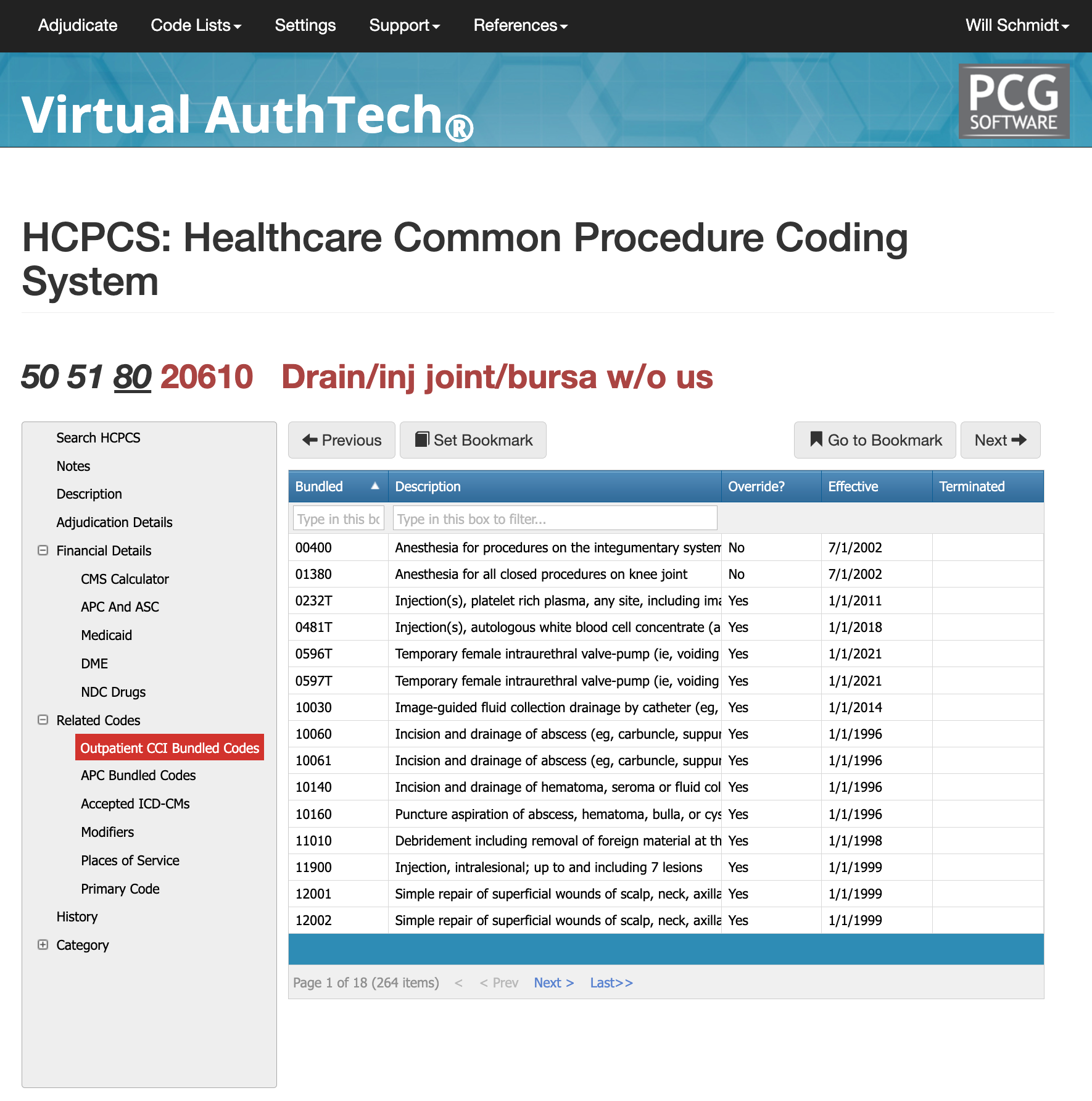
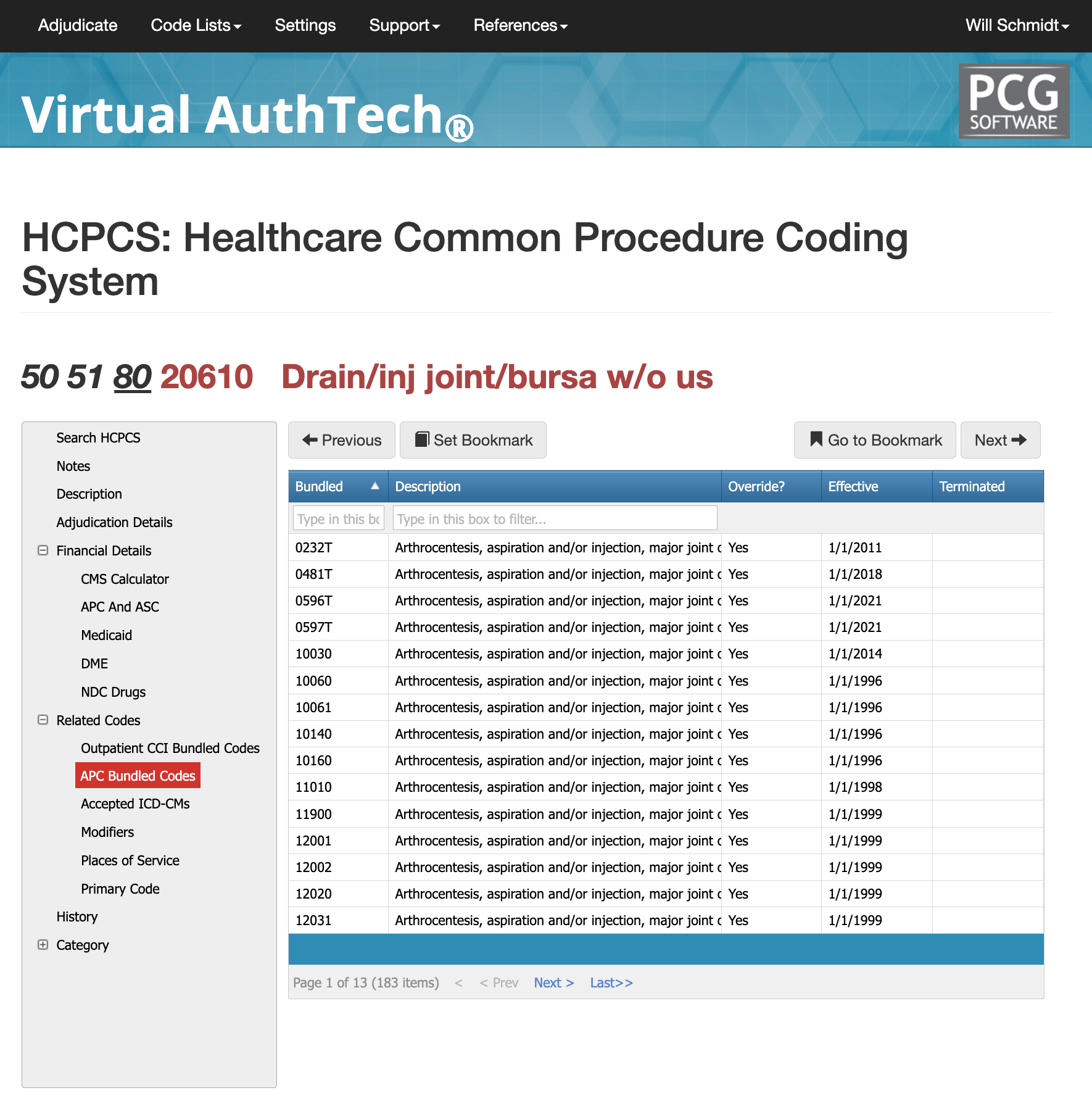
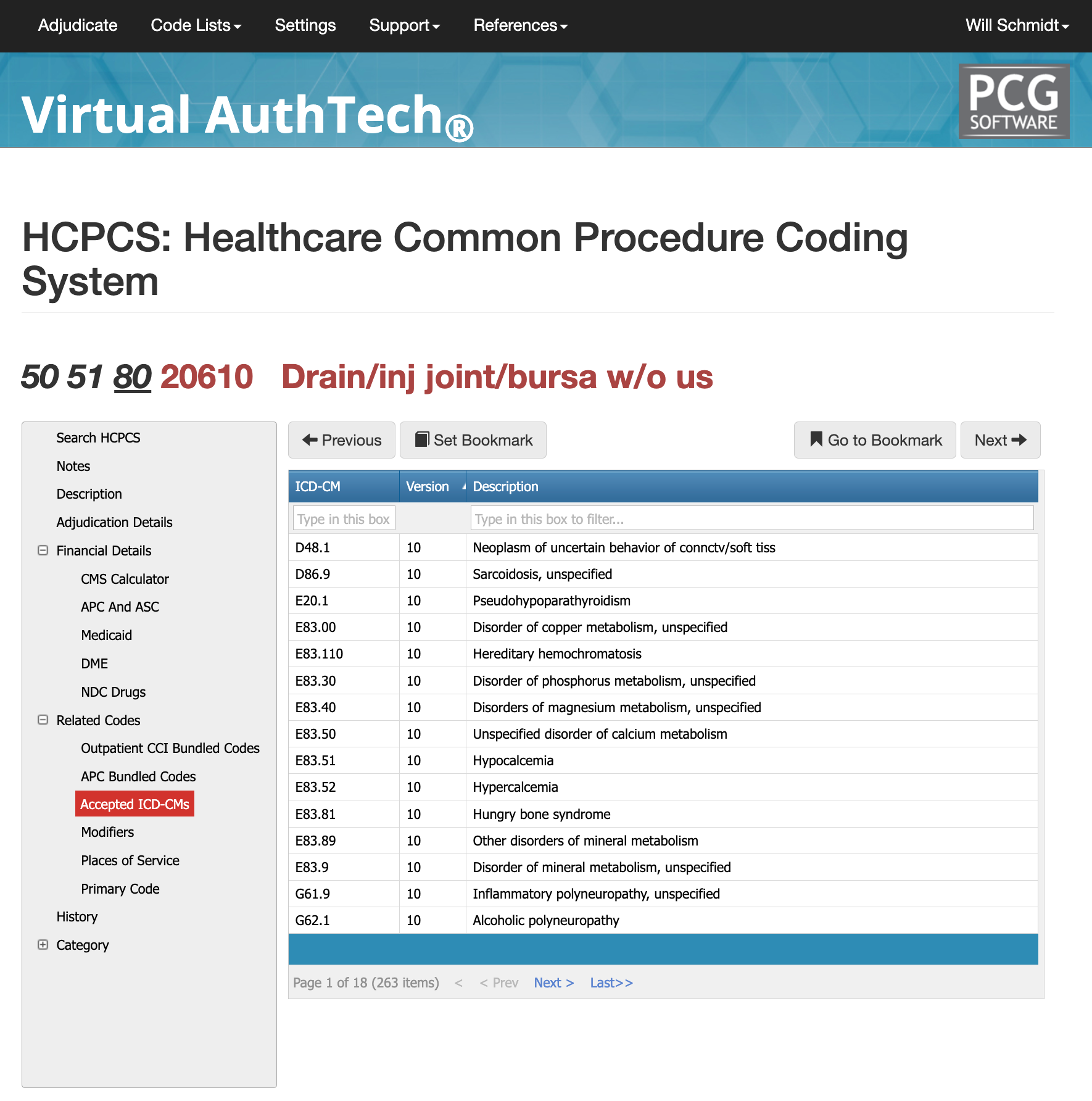
Related Codes for CPT Code 20610
There 264 related outpatient CCI Bundled Codes to 20610 CPT, 183 APC Bundled Codes, and 263 ICD codes as well. You would need to review the claim to be submitted along with clinical documentation against VA's database to ensure that the code you are billing is allowed and compliant. (see below as an example).
Places of Service for 20610 CPT Code:
- Physician Offices: Most commonly used in outpatient settings where orthopedic specialists, rheumatologists, or pain management doctors perform joint injections or aspirations to treat conditions like arthritis, bursitis, or joint effusion.
- Ambulatory Surgical Centers (ASCs): In outpatient surgical settings, where joint procedures are done under local anesthesia, often for more complex cases or when additional interventions are required.
- Hospitals (Outpatient Departments): Hospitals with outpatient departments or musculoskeletal clinics may also perform these procedures, especially if the patient requires more extensive monitoring or has underlying health concerns that require a hospital setting.
- Orthopedic Clinics: Often performed by orthopedic specialists to treat musculoskeletal conditions, including joint injuries, arthritis, or tendinitis.
- Pain Management Clinics: Used to manage chronic pain conditions by injecting corticosteroids or other medications into the joints or bursae to reduce inflammation and provide pain relief.
Modifiers for CPT Code 20610
Modifier 50: Bilateral Procedure
- Usage: Modifier 50 is used when a procedure is performed on both sides of the body during a single session. For CPT code 20610, if the aspiration or injection is performed on both joints or bursae, for example, both knees or both shoulders, modifier 50 would be added to indicate that the procedure was done bilaterally.
- Example: If a patient requires joint injections in both knees, code 20610 would be billed with modifier 50 to indicate it was performed on both knees in the same session.
- Reimbursement: The reimbursement for bilateral procedures is often higher because it covers both sides, although some payers may reduce the amount based on their specific billing policies.
Modifier 51: Multiple Procedures
- Usage: Modifier 51 is used when multiple procedures are performed during the same session. This modifier would be applied to CPT code 20610 if it is performed along with other procedures during the same encounter.
- Example: If a patient is receiving an injection into the knee and shoulder, both procedures may be billed with their respective CPT codes (e.g., 20610 for the knee injection and another CPT code for the shoulder procedure). Modifier 51 would be added to the second and subsequent procedures to indicate that they were performed together during the same session.
- Reimbursement: When modifier 51 is used, the second and subsequent procedures are typically reimbursed at a reduced rate, based on the payer's policies.
Modifier 80: Assistant Surgeon
- Usage: Modifier 80 is used to indicate that an assistant surgeon was involved in the procedure. This modifier is applied when an assistant surgeon is required to help with the procedure, usually for more complex or lengthy interventions.
- Example: If the procedure requires an assistant to help with the joint injection or aspiration (for example, to hold the joint in place or assist in more intricate techniques), modifier 80 would be added to the CPT code 20610 to indicate the presence of an assistant surgeon.
- Reimbursement: The use of modifier 80 generally results in additional payment to the assistant surgeon, typically a percentage of the primary surgeon's fee. The specific percentage depends on the payer's policies.
Need Daily Help with codes like 20610?
While information blogs like this are helpful, we caution against the usage of AI chatbots like ChatGPT to get your coding guidelines or answers. Virtual AuthTech is a real-time research tool that is part of a payer's daily auditing and claims process we call Virtual Examiner. If you're looking for advanced claims auditing, please contact us today by clicking here.
Will Schmidt joined PCG Software as their Chief Strategy Officer in November 2022. Prior to PCG, Schmidt lead TNH as their Sr. Vice President to become the 7th largest pharmacy in the nation. He then went on to consult with and serve as Interim CEO or Consultant to over 20 different companies specializing in profit strategies, operational efficiencies, vendor relations and partnerships, and exit strategies, include an international Revenue Cycle Management Company.
Our History and Credibility in Reporting this Information:
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.