10 Compelling Reasons to Embrace AI Medical Coding Software for Higher Approval Rates, Cleaner Claims, and Faster Collections
Background:
In the ever-evolving landscape of healthcare, where precision, efficiency, and accuracy are paramount, the integration of artificial intelligence (AI) has emerged as a transformative force. One critical area where AI's potential shines brightly is healthcare billing. As practice managers and revenue cycle managers of medical clinics, your pursuit of higher approval rates, cleaner claims, and faster collections can be greatly enhanced through the adoption of AI medical coding software. In this article, we delve into ten compelling reasons why embracing AI medical coding software, such as iVECoder, is not just a strategic move, but a necessity.
Internal Case Study using iVECoder to predict the usefulness of AI in healthcare billing for years to come
The future of AI in healthcare billing promises to revolutionize the entire reimbursement landscape, offering a more efficient, accurate, and streamlined process for healthcare providers and insurers alike. AI's potential to automate and optimize various billing tasks is poised to significantly reduce administrative burdens, mitigate billing errors, and expedite the reimbursement cycle.
One of the key areas where AI is expected to make a profound impact is in coding and documentation. Natural language processing (NLP) algorithms can parse through clinical notes, extracting relevant information and converting it into accurate billing codes. This not only saves time for medical coders but also reduces the risk of human errors that often lead to claim denials or delays. Moreover, machine learning models can continuously learn from historical claims data, adapting to evolving coding guidelines and ensuring compliance with regulations.
AI-driven predictive analytics are set to enhance revenue cycle management. By analyzing patterns in patient behavior, treatment plans, and claim histories, AI algorithms can anticipate potential discrepancies or discrepancies in billing, helping providers proactively address issues before claims are submitted. This preemptive approach minimizes costly denials and appeals while optimizing the revenue stream.
Another significant application lies in fraud detection. AI-powered systems can identify irregularities and anomalies in billing patterns, potentially uncovering instances of fraudulent claims or overbilling. By cross-referencing vast datasets and identifying outliers, AI tools can alert healthcare institutions to investigate suspicious activities, safeguarding the integrity of billing processes and reducing financial losses.
Furthermore, AI's ability to enhance patient engagement and transparency is noteworthy. Chatbots and virtual assistants powered by AI can address patients' billing inquiries promptly, improving overall satisfaction. These tools can also provide personalized cost estimates for medical procedures, empowering patients to make informed decisions about their healthcare choices.
Nonetheless, as AI becomes more integrated into healthcare billing, ethical considerations must be taken into account. Ensuring data privacy and security, preventing bias in AI algorithms, and maintaining a balance between automation and human oversight are paramount.
1. Enhanced Accuracy and Precision
Manual medical coding is prone to errors, leading to claim denials and revenue loss. AI medical coding software eliminates this risk by leveraging machine learning algorithms that continuously learn from vast datasets. This results in heightened accuracy and precision in code assignment, minimizing claim rejections due to coding errors.
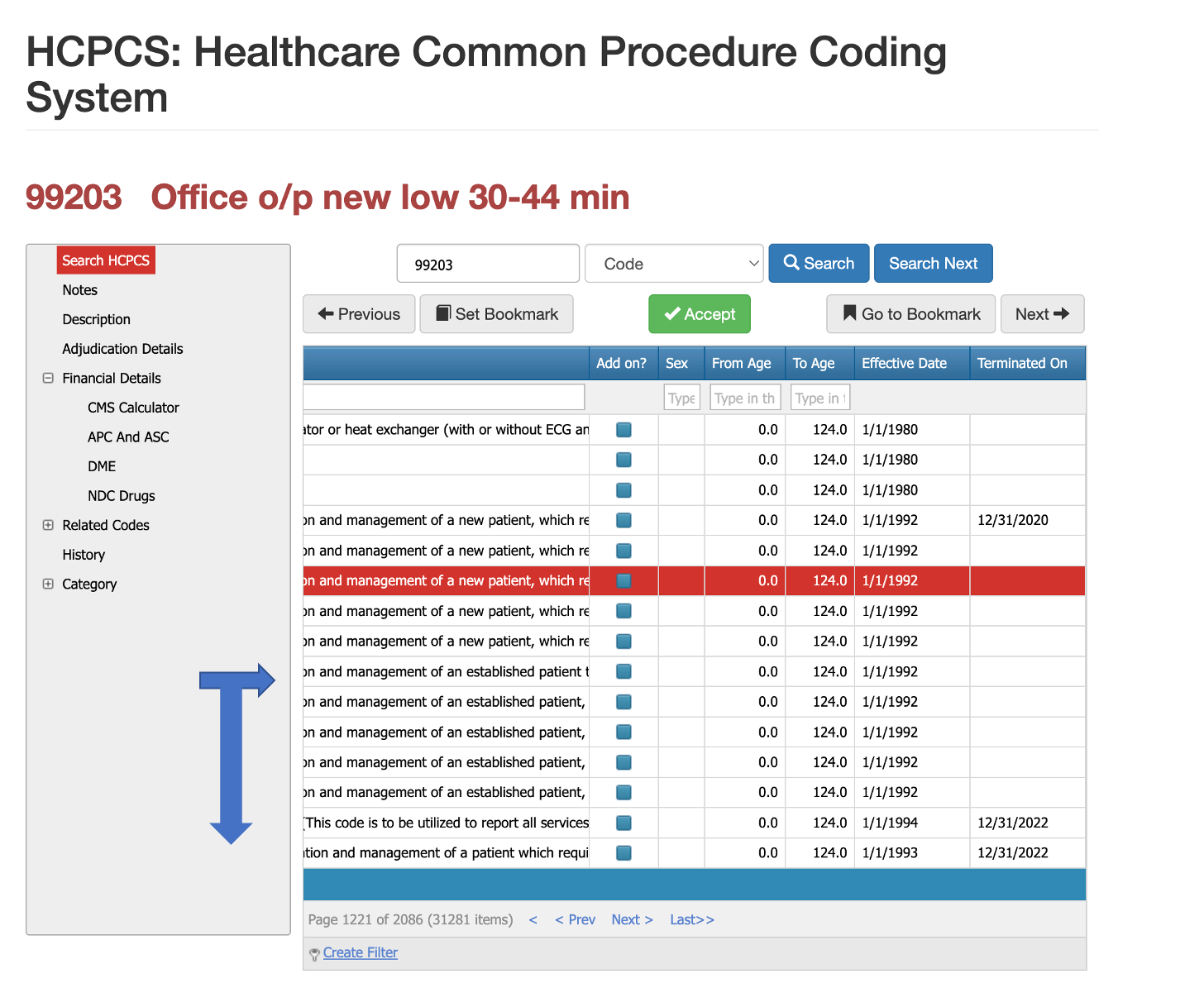
2. Real-time Coding Guidance
AI Medical Coding softwares like iVECoder offer real-time coding guidance based on the latest industry standards and regulations. It ensures that your claims are aligned with the most up-to-date coding rules, reducing the likelihood of denials due to outdated or incorrect codes.
3. Increased Approval Rates
AI medical coding software like iVECoder can significantly boost approval rates by suggesting the most appropriate codes for complex medical procedures. Its intelligent algorithms analyze patient records, treatment descriptions, and documentation to ensure accurate code selection, ultimately leading to higher claim approval rates.
4. Efficient Resource Allocation
By automating the medical coding process, your team can redirect valuable resources towards higher-value tasks such as patient care and revenue optimization. This streamlining of administrative tasks contributes to a more efficient workflow and improved clinic performance.
5. Comprehensive Claim Reviews
iVECoder's AI-driven capabilities allow for thorough claim reviews before submission. It scans for potential errors, discrepancies, or missing information, enabling you to submit cleaner claims that are less likely to face scrutiny or rejection.
6. Faster Reimbursements
With AI medical coding software, the coding process becomes quicker and more streamlined. This expedites the claims submission timeline, leading to faster reimbursements and improved cash flow for your medical practice.
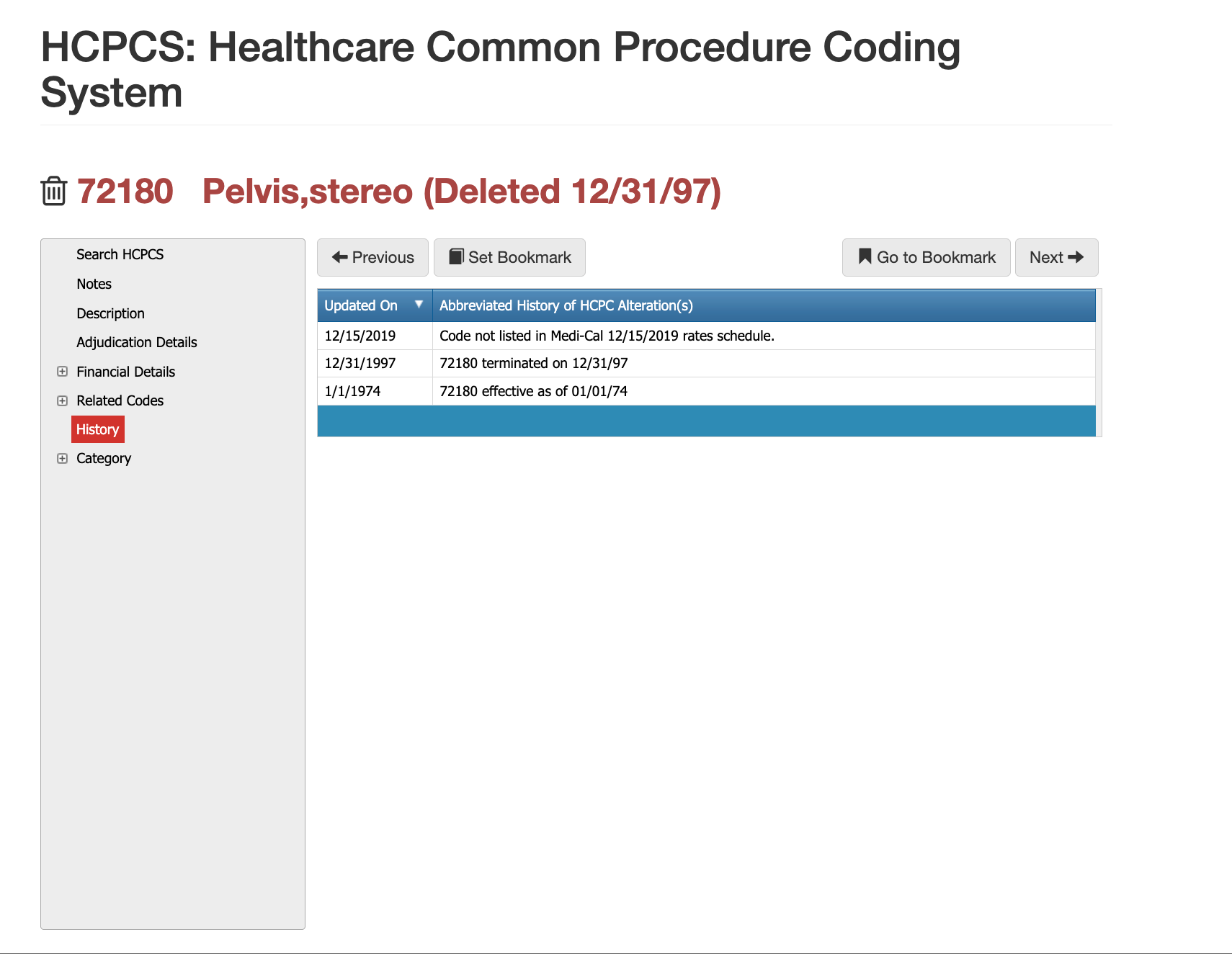
7. Adaptation to Industry Changes
The healthcare billing landscape is constantly evolving, with new codes and regulations introduced regularly. AI medical coding software is designed to adapt swiftly to these changes, ensuring that your claims remain compliant and accurate even in the face of dynamic industry shifts.
8. Reduced Compliance Risks
Coding errors can inadvertently result in compliance breaches, leading to legal complications and financial penalties. By leveraging AI medical coding software's meticulous accuracy, you can minimize compliance risks and safeguard your clinic's reputation.
9. Data-Driven Insights
AI medical coding software generates valuable insights from the coding and billing process. These insights provide a deeper understanding of reimbursement patterns, common denial reasons, and revenue trends, empowering you to make informed strategic decisions for your practice.
10. Improved Patient Satisfaction
Efficient billing processes contribute to a seamless patient experience. When claims are processed accurately and promptly, patients encounter fewer billing-related issues, leading to higher satisfaction rates and stronger patient-provider relationships.
CMS includes Stakeholders for increased buy-in
In conclusion, the integration of AI medical coding software, exemplified by iVECoder, offers a myriad of benefits to practice managers and revenue cycle managers seeking higher approval rates, cleaner claims, and faster collections. From enhanced accuracy and real-time guidance to increased approval rates and streamlined processes, the impact of AI on healthcare billing is undeniable. As technology continues to reshape the healthcare landscape, staying ahead of the curve by adopting innovative solutions like iVECoder is not just a competitive advantage—it's a necessity.
Experience the Future with iVECoder
Are you ready to revolutionize your healthcare billing processes? Discover the transformative power of AI medical coding software with iVECoder. Say goodbye to claim denials, errors, and delays, and say hello to higher approval rates, cleaner claims, and faster collections. Explore iVECoder today and elevate your medical practice to new heights.
Learn more about iVECoder by
CLICKING HERE
Our History and Credibility in Reporting this Information:
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.