#1 AI Medical Claims Auditing Software for Health Plans, MSOs, PACE, TPAs, and CCOs
Virtual Examiner®
Imagine walking into work tomorrow and having a complete list of claims that shouldn't be paid, that should be reduced, and every reason clearly explained.
✅ 100% Compliance Possibilities
✅ 100% Auditing Potential
✅ 72 million + Edits
✅ Quarantines Claims over Night
✅ Fraud, Waste, Abuse
✅ NCCI, CMS, Medicaid
✅ Customizable Edits
✅ Free Audits and Demos
AI Claims Auditing for Payers
What is Virtual Examiner®
AI Claims Editor with Reason Codes Serves as Instructor to Employees
Imagine saving millions every year, cleaner encounter data, and happier claims examiners with the usage of Virtual Examiner®. Every night it will audit the days claims, quarantine those claims based on a 3-year full episode of care audit, and then tell you every possible reason to deny, reduce, or pend for contractual review, all based on CMS and AMA guidelines. Virtual Examiner® will not only tell you why a claim should be denied, the CMS definitions and coding suggestions, as well as a layman’s term of what the information provided means. It’s not just a Claims Editor or Claims Auditor, it’s a guiding tool to optimizing your Claims Department process and helpful in onboarding new employees.
Cost Containment
Operational Efficiency
Compliance
Modules and Benefits of Virtual Examiner®
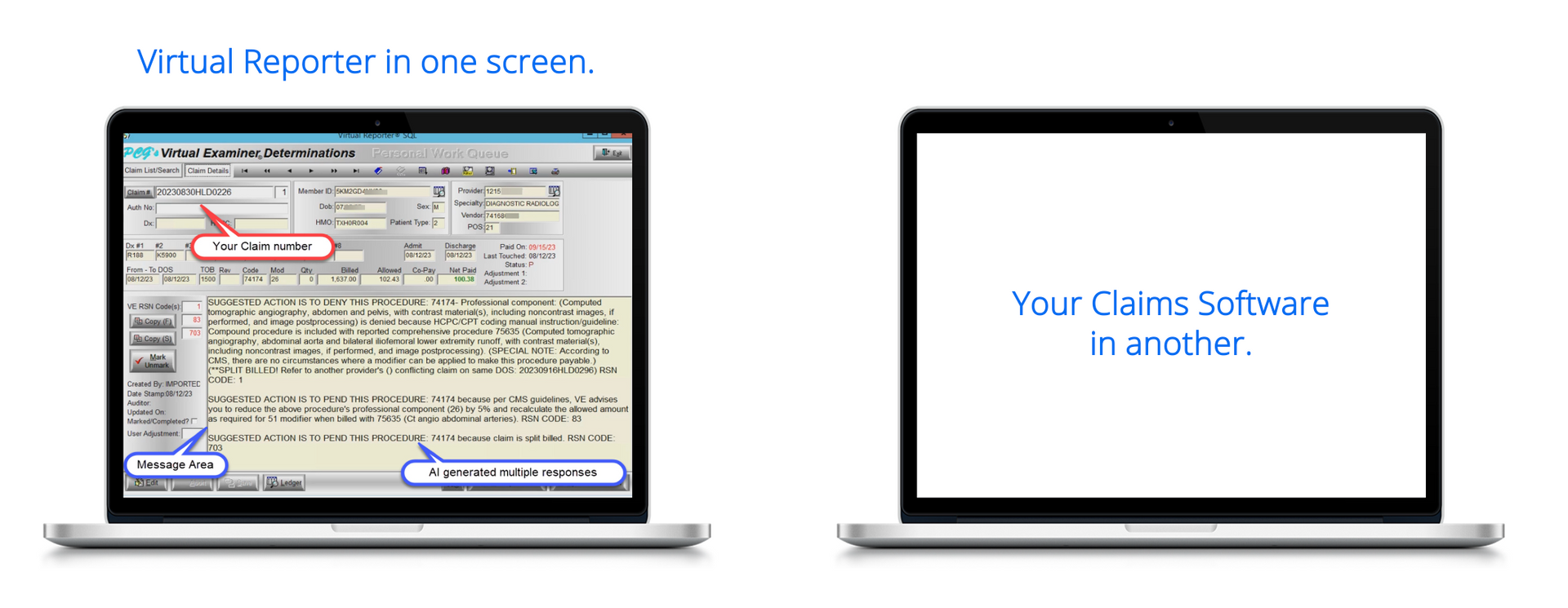
Virtual Reporter® - VR
Increased Efficiency of Claims Department
Our AI Engine, Virtual Examiner® has a reporting module called Virtual Reporter®. Every night Virtual Reporter® will run all of your unpaid claims against the latest CMS, AMA, and State Medicaid guidelines and your pre-set exclusions. When your team comes into work the next day, they have reports of only the claims that have one of 400 possible reason codes for denial. Your team can then review those claims and find the reasons for each suggested denial or pending, and not only make that decision but also learn from the reason codes for faster future reviews and decision making.
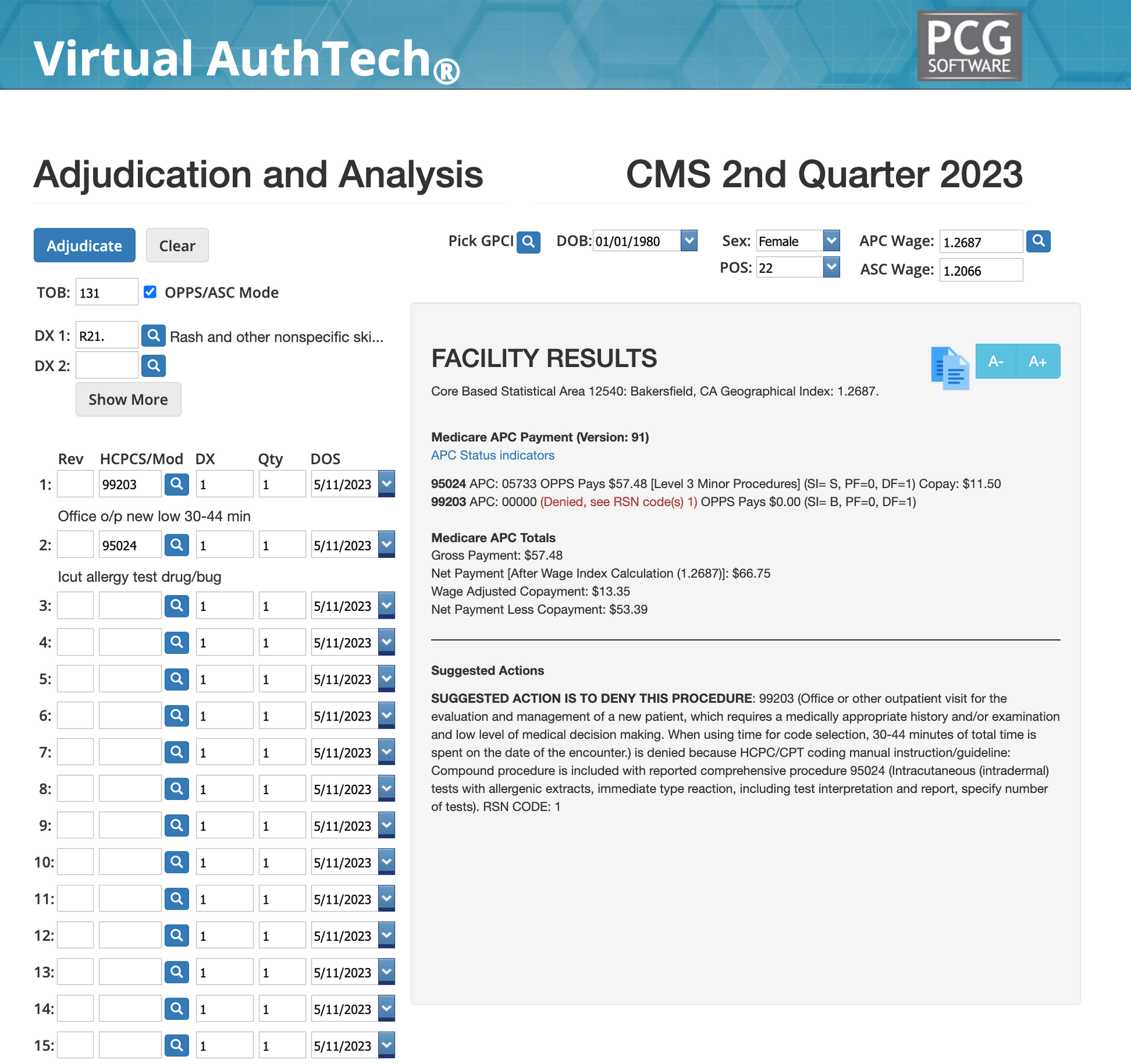
Virtual AuthTech® - VA
The Clear Claim Connection
The Perfect Claims Audit Tool
With your new Virtual AuthTech® module, your Medical Management and Authorizations teams will be equipped to review complex authorizations and run mock adjudications to avoid erroneously approving claims that are not medically necessary, fall under a CCI edit, or hundreds of other reasons to which Virtual AuthTech® within it’s Machine Learning AI Knowledge base will advise you on next steps.
SymKey® Virtual Auto-Posting
Claims Automation AI
PCG and your IT Department will work hand in hand to identify the possibility of auto-adjudication with Virtual Examiner® and your current in-house or commercial recognized claims software already in place. Integrations can lead to auto-posting capabilities, expedited speed in AI claims tasks, AI generated tracking of retro-rate reconciliation, AI generated eligibility review, AI generated co-pay / co-insurance correction, and can be installed in a single day.
SymKey is a registered trademark owned by HealthCare Information Management, Inc (HCIM) and integrates with Virtual Examiner® To get a listing of integrated systems book a FREE consult with PCG.
FREE Comprehensive AI Medical Claims Audit
Guaranteed ROI and Data on Future Cost Containment
In less than 10 days, PCG’s Claims Expert and Virtual Examiner® will conduct a full 3-year claims analysis identifying codes and processes that produced overpayments and claims that should have never been paid in the first place. Your Audit will show you how to reduce risk, what to recover first, and what to immediately address with your teams. Lastly, we go over how we make our Claims Editor, Auditor, Authorizations Tool, and Support, provide you an ROI in 90 days or less from a signed contract. This full report is shown to you, your claims team members, and decision makers at your headquarters. This entire auditing process is valued at $50,000 but we're willing to do this for FREE if both parties agree to the audit.
Knowledge is Power
What does your data tell you?
Virtual Examiner is your Data Analyst, Compliance Officer, and CMS and AMA Expert, all rolled into one.
- Top 40 unbundling by group
- Top 40 unbundling by provider
- Double Billing
- Improper and Fraudulent usage of Modifiers
- Improper or Abusive Medication Prescribing
- Place of Service errors
- Billing submission frequency, aka "Spiking"
- E&M graph provider and group error trends.
- Every code, every scenario, its there for you!
And about a million other things we'll get into during our FREE Consult
Virtual Examiner Client Support Programs
Virtual Examiner® Implementation
At PCG, we believe in Clients first. That’s why we fly out to your headquarters, train your claims and medical management teams, your provider relations, and your fraud, waste, and abuse teams. While we’re training you and your team, we’re also training on live claims that require editing and denials pre-check runs and paid claims that require review and recovery. PCG and Virtual Examiner save you money from Day 1.
Virtual Examiner® Support Team
Once we get your team live, you have the full support from our IT Team, our Certified Professional Coders, Nurses on Staff, and even our Executives. We are a hands on, results and support driven company.
PCG Newsletter
All Virtual Examiner® (VE) and VEWS clients of PCG get our quarterly Newsletter and regular updates on the latest Code Edits, Lawsuits, and Tactics for higher profitability. The PCG Newsletter is also located within Virtual AuthTech® and can be downloaded at any time.
Provider Relations: Operation Clean Claims
PCG Software’s Virtual AuthTech® has a twin sister that we call iVECoder ® that can be used by clinics to submit cleaner claims. Our CSO would happily walk your provider relations through your provider letters, outreach and possibly iVECoder adaption.
FAQs about Virtual Examiner®
Asked and Answered Common Questions about Virtual Examiner®
Case Studies of Success
Monarch Health Systems
Customizable work queues saves them $160,000 or more every month!
Naperville Healthcare Associates
Physician-hospital organization saw a 56 percent savings increase on fee-for-service claims. Read full story
Tuality Health Alliance
Physician-hospital community organization with 300+ providers reduced 10% of overpaid claims in year 1. Read full story
Physicians Integrated Medical Group
Within 30 days of implementing Virtual Examiner, PIMG had already saved $30,000 in overpaid claims during their audit. Ready full story